The benefit of shoulder arthroplasty is measured by the preoperative to postoperative change in shoulder comfort and function as perceived by the patient. When preoperative scores are not obtained, it is tempting to try to "retrieve" the preoperative state of the shoulder from the patient's memory.
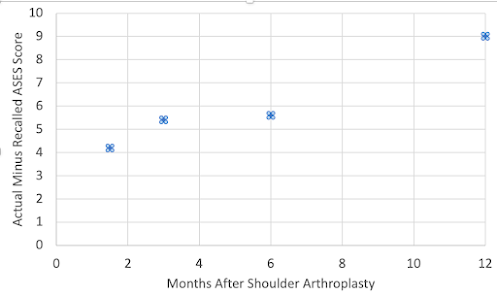
These authors investigated the accuracy of patient recall in determining the preoperative American Shoulder and Elbow Surgeons (ASES) score for patients having total shoulder arthroplasty (TSA). They compared actual ASES scores determined prior to surgery with ASES scores based on patient recall at at 6 weeks, 3 months, 6 months, and 12 months after surgery.
They divided the ASES score into two subcomponents: functional ability and visual analog scale (VAS) for pain.
While recalled ASES function scores were comparable to corresponding preoperative scores across
all time points (analysis of variance, P = .21), recalled VAS pain was significantly higher at all time
points beyond 6 weeks after surgery.
As a result, the recalled preoperative total ASES score was worse than the measured preoperative score.
This indicates that the benefit of shoulder arthroplasty (preoperative to postoperative change) based on recall of the preoperative condition of the shoulder is likely to be exaggerated. Therefore, measurement of the benefit of shoulder arthroplasty needs to be based on the actual, rather than the recalled preoperative comfort and function of the shoulder.
Comment: The results of this study also create uncertainty about the commonly used "anchor method" for determining the minimal clinically important difference (MCID). The "anchor"is often a questionnaire that asks patients to rate retrospectively the improvement in their shoulder after shoulder arthroplasty. For example, a 4-point anchor might ask patients to rate the change in pain after surgery as “worse,” “no different,” “improved,” or “much improved.” The MCID for the ASES score would be the difference in the average ASES scores of patients answering “worse” or “no change” and the average ASES scores of patients who answered “improved.” Because this study found that patients inaccurately recalled their preoperative pain, their ability to rate the amount of change in pain may also be inaccurate. Specifically, if patients recall more pain than they actually had, some patients may rate their shoulder as "improved" whereas the actual change in pain was "unimproved".
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
How you can support research in shoulder surgery Click on this link.
Here are some videos that are of shoulder interest