These authors analyzed a series of 264 reverse total shoulders (RTSAs) to determine
the influence of preoperative opioid use on clinical and radiographic outcomes at a minimum of 2 years’ follow-up. 71 (27%) of these patients were classified as preoperative opioid users by applying of the Centers for Disease Control and Prevention definition: ≥3 months of opiate use prior to surgery excluding atypical opioid medication (eg, tramadol).
There were substantial preoperative differences between the two groups other than their use of narcotics as shown below.
Postoperatively, opioid users had significantly inferior visual analog scale pain scores (2.59vs. 1.25), American Shoulder and Elbow Surgeons scores (63.2 vs. 75.2), active forward elevation, and internal and external rotational shoulder strength compared with opioid-naive patients.
However, the difference between the followup and preoperative ASES scores (i.e. the amount of improvement) was identical for the two groups. Thus if outcome is defined as the change in score from before to after surgery, the outcomes for the opioid users were not inferior to the non-users.
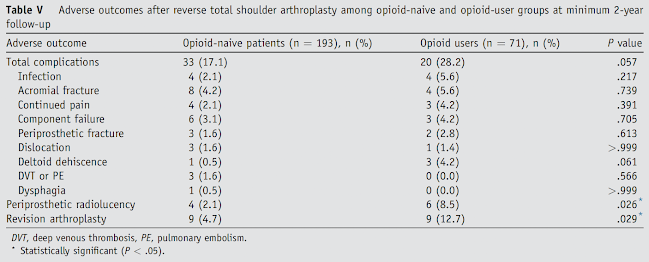
There were differences between groups in the rates of postoperative adverse events, most of which were not statistically significant.
Comment: In this study a substantial number of patients having RTSA met the definition of "opioid user". Of note this definition lumps patients taking 5 mg of Oxycodone each evening with those taking much higher doses. It does not distinguish patients taking medication for their shoulder from those taking it for other reasons (e.g. low back pain). The paper did not determine whether the patients' narcotic use diminished after RTSA.
Nevertheless, the data indicate that on average ASES scores can be improved after RTSA in each group by an amount exceeding the published values for the minimal clinically important difference (MCID) (between 9 and 20.9 points). Using the lower MCID cutoff for the ASES score, 84.5% of opioid-naive patients (163 of 193) and 85.9% of opioid users (61 of 71) reached a clinically significant improvement in the ASES score.
In our practice we pay careful attention to all prescription and non-prescription medications taken by patients being considered for arthroplasty, including the dosage, the reasons for the medications and the provider prescribing the medication. For those taking more than a trivial amount of narcotics, we make sure the patient understands that those who are not opiate naive may have increased difficulty with postoperative pain management. In these patients we require identification of a provider other than the surgeon who agrees to manage the narcotic medication postoperatively, warning the patient that - while it is hoped that the procedure will reduce their shoulder pain in the long run - the immediate postoperative pain may be greater than that experienced before surgery.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/