Hospital satisfaction does not predict functional outcome one year after total shoulder arthroplasty
These authors point out that currently 2% of Medicare reimbursements is linked to value measures including the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) hospital satisfaction survey. In this study they sought to determine whether HCAHPS survey results correlated with patient self-assessed measures of comfort and function in 84 patients undergoing elective total shoulder arthroplasty.
Patients were contacted by a third-party survey company between 48 hours and 6 weeks after hospital discharge to complete the HCAHPS survey by telephone. All patients enrolled in this study were attempted to be contacted one time by the survey company to complete the HCAHPS survey.
Patients completed the ASES and WOOS questionnaires by mail or online at the 3-month and 1-year post-operative time points. They were also asked to complete a self-reported satisfaction questionnaire about how effective surgery was in improving pain and function (0–10 ordinal scale). Patients who failed to complete the enrollment packet, HCAHPS survey, or the 1-year ASES follow-up survey were excluded from the analysis.
Approximately 200 patients were approached for study enrollment of which 163 consented to participation. Of these 84 patients completed the necessary forms for inclusion in the study.
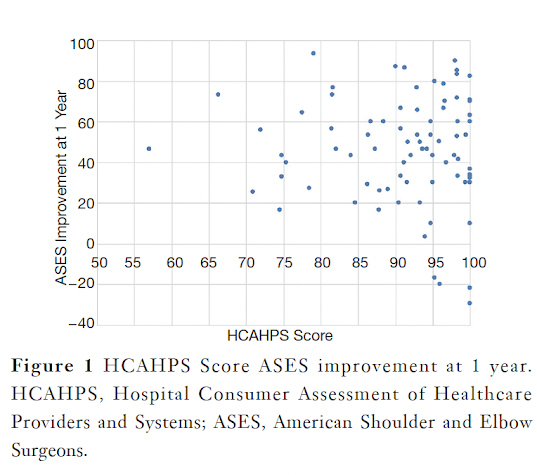
As can be seen below, the HCAHPS score is based on questions related to the process of care rather than the functional outcome.
The average ASES scores improved by 45 points from 36 before surgery to 82 at one year. The HCAHPS scores ranged from 57 to 100
As can be seen from the above chart, the HCAHPS scores were not correlated with ASES (r=0.09, P=0.44) at one year after surgery. HCAHPS was also not correlated with the absolute improvement in ASES (r=−0.02, P=0.85) from pre- to one year post-operatively.
The single question “How effective was the surgery in restoring a normal level of function?” at three months after surgery showed high correlation with improvements in ASES score (r=0.38, P=0.001) at the one-year post-operative time point. Similarly, the question “How helpful was the surgery in relieving pain?” at three month post-operatively was associated with improvements in ASES (r=0.43, P<0.001) scores at one year after surgery. Neither the function question (r=0.21, P=0.07) nor the pain question (r=−0.06, P=0.62) at three months was correlated with HCAHPS scores.
Comment: This is an interesting study indicating that the 2 day to 6 week post op HCAHPS score did not correlate with improvement in comfort and function at 1 year. The HCAHPS is based on patient-nursing interactions, patient-doctor interactions, hospital environment, and pain management, As might be suspected, recollection of these characteristics would be fresh in the patient's mind soon after discharge ("the bathroom was clean/dirty", "the nurses brought my pain meds promptly/late"). On the other hand, at a year after surgery the patient's mind is more likely to be focused on improvement in and current function of the shoulder. Thus it is not a surprise that the two metrics which measure different things at different times would be discordant. It would be of interest to obtain an HCAHPS score at one year to compare with (1) the ASES score at one year and (2) the HCAHPS immediately after surgery. It seems likely that the recollection of a dirty bathroom would subside in the presence of a comfortable functional shoulder.
The authors point out that under CMS procedures, reimbursement to hospitals is directly affected by survey results which in turn may directly or at least indirectly affect providers in some health care models.
As far as we know, there are no direct Medicare incentives for improving shoulder comfort and function, yet that is presumably the reason patients have shoulder arthroplasty to begin with (not to have a pleasant hospital stay).
The author of What Switching to Value-Based Care from Fee-for-Service Reimbursement Means for Healthcare Providers states, "The transition to value-based care revolves around a recalibration of how healthcare is measured and how payments are reimbursed. The traditional model, known as fee-for-service, simply assigns reimbursements based on what services a healthcare organization provides. But in value-based care, reimbursement is contingent upon the quality of the care provided and it comes tethered to patient outcomes." The authors of Hospital satisfaction does not predict functional outcome one year after total shoulder arthroplasty point out that current measures of the quality of patient care (vis HCAHPS) are NOT, in fact, "tethered to patient outcomes".
At present, the incentives for surgeons to safely improve the comfort and function of patients with shoulder arthritis via shoulder arthroplasty are patient gratitude ("you gave me back a shoulder that works and is comfortable") and surgeon satisfaction ("I did good"). For now, that's plenty. Meanwhile, we will continue to urge our medical centers to support our efforts to provide a good patient experience.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
How you can support research in shoulder surgery Click on this link.
Here are some videos that are of shoulder interest