Wear, loosening, and migration of the prosthetic glenoid component can complicate anatomic total shoulder arthroplasty.

Polyethylene wear can cause osteolysis of the bone around the glenoid and humeral components leading to insufficient bone stock and bone quality for re-implantation.
Although there is a trend to manage failed anatomic total shoulder arthroplasties (aTSA) with revision to a reverse total shoulder arthroplasty, such revisions can be complicated by introperative fracture, difficulties in baseplate fixation, postoperative component loosening, instability, infection, neurologic injury and acromial or scapular spine stress fractures.
Some cases of failed aTSA can be successfuly revised to a hemiarthroplasty (HA).
The authors of Revision of total shoulder arthroplasty to hemiarthroplasty: results at mean 5-year follow-up investigated the outcomes reported by patients after conversion from aTSA to HA. Intraoperative glenoid or humeral component loosening was found in all 29 patients.
76% of the patients were satisfied with the procedure. Pain improved in 87% of the patients with mean pain scores improving significantly from 6.2 to 3.1. Simple Shoulder Test (SST) scores improved from a mean of 4.1 to 7.3. 62% had improvement exceeding the SST MCID threshold of 2.4. No significant differences in patient or shoulder characteristics were found in comparing those patients who improved by an amount greater than the MCID of the SST to those patients who improved less than the MCID. However, among the 6 patients who underwent conversion from aTSA to HA with cuff failure, only 3 (50%) attained MCID improvement of SST and 3 (50%) were satisfied with their revision.
59% of the patients had ≥2 positive cultures with the same bacteria; 82% of these were with Cutibacterium. Thus obtaining cultures at the time of revision is important. Furthermore, in view of the observation that over half of the revisions met the definition of having a periprosthetic infection (even though there were no obvious preoperative signs of infection), surgeons should consider complete, rather than partial, single-stage exchange and postoperative antibiotic therapy. Seven (88%) of the 8 patients with a loose humeral component had ≥2 positive cultures with the same bacteria. Surgeons should have an even higher index of suspicion for infection in cases of humeral component loosening.
Four patients (14%) required conversion to total shoulder arthroplasty: 2 to anatomic and 2 to reverse. An additional 3 patients (10%) had a revision HA performed because of persistent pain and stiffness.
There were no intraoperative fractures, problems with component fixation, infections, neurologic injuries or scapular stress fractures.
Comment: While the technique for revision of a failed total shoulder to hemiarthroplasty is not discussed in this paper, there are several options to be considered.
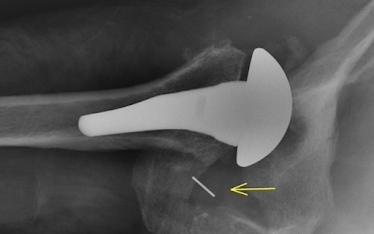
(1) Humeral head component removal, retention of a securely fixed humeral stem, glenoid component removal, debridement, culturing of deep tissue and explants for Cutibacterium, smoothing of the residual glenoid bone, insertion of a new humeral head with modifications of eccentricity, head diameter of curvature, and head thickness as needed to balance the shoulder's smoothness, mobility and stability, followed by a course of antibiotics until the results of the cultures are finalized. Some case examples of this method are shown below. In the case on the left, note the use of an inferiorly excentric humeral head component. In the case on the right, note the upsizing of the diameter of curvature to help distribute the load to the rim of the remaining glenoid bone. Glenoid bone grafting was not used in these cases.
(2) Complete single stage exchange with humeral head and body removal, glenoid component removal, debridement, culturing of deep tissue and explants for Cutibacterium, smoothing of the residual glenoid bone, insertion of a new body and a humeral head with eccentricity, head diameter of curvature, and head thickness as needed to balance the shoulder's smoothness, mobility and stability, followed by a course of antibiotics until the results of the cultures are finalized. The case for this approach is based on the observation that over 50% of cases in this study had culture evidence of periprosthetic infection (PJI), even in the absence of preoperative signs of infection. The problem is that the results of the cultures are not available in time to influence the surgical decision or the decision about antibiotics immediately after surgery. Complete single stage revision would seem to be particularly indicated in cases of humeral component loosening in view of the even higher association with PJI. (see Single-Stage Revision Is Effective for Failed Shoulder Arthroplasty with Positive Cultures for Propionibacterium). See the illustrative case below.
(3) Primary conversion to a reverse with removal of humeral head and body removal, glenoid component removal, debridement, culturing of deep tissue and explants for Cutibacterium, smoothing of the residual glenoid bone, insertion of a reverse total shoulder followed by a course of antibiotics until the results of the cultures are finalized. This approach would seem to be most applicable to shoulders with combined prosthetic and rotator cuff failure - especially if the patient has pseudoparalysis. It should be undertaken with the recognition of a high complication rate as pointed out by the authors of Salvage reverse total shoulder arthroplasty for failed anatomic total shoulder arthroplasty: a cohort analysis
See this related paper What is the optimal management of a loose glenoid component after anatomic total shoulder arthroplasty: a systematic review, that discusses four types of revision: hemiarthroplasty, 1-stage TSA, 2-stage TSA, and RSA, each of which had as high as a 20% re-revision rate!
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).





