In the first, Reaching MCID, SCB, and PASS for ASES, SANE, SST, and VAS following Shoulder Arthroplasty Does Not Correlate with Patient Satisfaction, the authors attempted to correlate patient satisfaction with previously defined values for minimal clinically important difference (MCID), substantial clinical benefit (SCB), and patient acceptable symptomatic state (PASS) for ASES, SANE, SST, and VAS at 2 years following shoulder arthroplasty for 352 patients.
They point out that historically the thresholds for MCID, SCB and PASS were established based on anchoring questions that did not account for patient satisfaction
In their study, satisfaction was assessed by a questionnaire asking: 1) on a scale of 1 to 10, what is your overall satisfaction with your surgical outcome? 2) if you could go back in time, would you undergo this operation again? (yes/no) 3) for the same condition, would you recommend this operation to a friend or family member? (yes/no).
ASES scores improved from 42 to 88, SANE improved from 36 to 87, SST improved from 5 to 10, and VAS improved from 5 to 1.
Mean patient satisfaction was 9.0. 94% of the patients would undergo surgery again
94% of the patients would recommend surgery.
12% of the patients reported satisfaction scores below 8 out of 10. This subset of patients had a mean ASES of 75, SANE of 71, SST of 8, and VAS of 2.
8 patients did not reach MCID for any of the outcome metrics, but 5 of these reported satisfaction scores of 8 or higher.
42 patients did not reach SCB in any of the four outcome metrics, but 28 of these reported satisfaction scores of 8 or higher.
24 patients did not reach PASS in any of the four outcome metrics, but 14 of these reported satisfaction scores of 8 or greater.
Spearman correlation coefficients were weak or very weak for reaching MCID, SCB, and PASS in ASES, SANE, SST, and VAS and all three study outcome metrics.
A second study, Anatomic Total Shoulder: Predictors of Excellent Outcomes at Five Years after Arthroplasty, reported minimum 5-year outcomes in patients undergoing TSA and sought to determine characteristics predictive of patients achieving an excellent functional outcome.
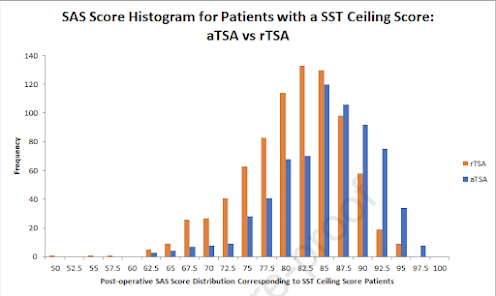
Preoperative demographic variables and Simple Shoulder Test (SST) scores were obtained pre-operatively and at a minimum of five years after surgery for 188 patients. A final SST ≥ 10 and percentage of maximal possible improvement (% MPI) of ≥ 66.7% were determined to be the thresholds for excellent outcomes.
Mean SST scores improved from 3 to 10. 62% and 71% of these patients achieved an excellent outcome as defined by five-year SST ≥ 10 and %MPI ≥ 66.7%, respectively.
Male sex and commercial insurance coverage were predictors of both SST ≥ 10 and %MPI ≥ 66.7. Workers' Compensation insurance was predictive of not obtaining SST ≥ 10 or %MPI ≥ 66.7).




The threshold for MCID was passed by the vast majority (95%) of patients undergoing TSA but did not necessarily indicate an excellent, satisfactory outcome.
The authors remind us that while the type of insurance is associated with patient outcome, the type of insurance coverage is a surrogate indicator for the patients’ social determinants of health. For example, patients having commercial insurance may be more likely to have higher levels of primary care, education, income, social support, as well as overall physical and mental health than patients covered by an alternative type of insurance. Each of those patient characteristics may be important factors affecting the outcome.
Comment: These studies point out that satisfaction is not strongly related to the absolute value of the amount of improvement. This makes sense: a patient improving from a preoperative SST sore from 2 to 6 will have exceeded the MCID, but still only can perform 6 of the 12 SST questions. Alternatively, an SST improvement from 9 to 11 would not exceed the MCID, but would indicate a shoulder that could perform 11 of the 12 SST functions.
A strong component of postoperative patient satisfaction is that the procedure met the patient's expectations of it. The observation that satisfaction is strongly correlated with an SST ≥ 10 and %MPI ≥ 66.7% indicate that the patient's expectation is that they will have a highly functional shoulder after arthroplasty (SST ≥ 10) and that most of their preoperative functional deficit will be mitigated by the procedure ( %MPI ≥ 66.7%).
This is valuable information for the arthroplasty surgeon. In patients who are unlikely to achieve SST ≥ 10 and %MPI ≥ 66.7%, it would seem prudent to inform them of this preoperatively - to set realistic expectations. Charles Neer understood this clearly; patients who were unlikely to achieve high levels of function were placed in a "limited goals" category and he carefully explained this reality to them before surgery.
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Contact: shoulderarthritis@uw.edu
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).