While reverse total shoulder can be a successful surgery for patients with pseudoparalysis, fracture and failed anatomic arthroplasty, the clinically ideal positioning and type of implant have yet to be determined. For example, while distalization of the glenosphere may lead to an increase in motion and lower risk for scapular notching, it comes with increased risk for neurological injury, acromial/scapular stress fractures and deltoid fatigue. Less distal positioning of the glenosphere may result in collision of the greater tuberosity against the acromion, with risk of loss of range of motion and acromial/spine fracture.
In an attempt to correlate component type and position with the rate of complications and clinical outcomes, many radiographic measurements have been proposed.
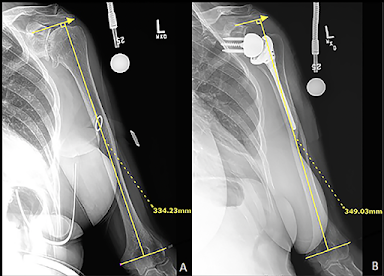
One example is "arm length" measurement - the distance between the transepicondylar line to the inferior aspect of the acromion. "Humeral lengthening" is the difference between this measurement before and after surgery.
Two other measurements are the lateralization shoulder angle (LSA below left) and the distalization shoulder angle (DSA below right)
It can be seen that these measurements do not directly reflect the position of the center of rotation nor the type or position of the humeral component. A recent article examined the clinical importance of these measurements.
Assessing the validity of the distalization and lateralization shoulder angles following reverse total shoulder arthroplasty
These authors explored the relationship between the distalization shoulder angle (DSA) and lateralization shoulder angle (LSA) and clinical outcome after reverse total shoulder arthroplasty performed in 238 patients by an individual surgeon.
One group had a 155 degree medialized design (Anatomical Shoulder Reverse System, Zimmer), 2.5 mm of lateral offset and a 36 mm glenosphere.
Another group had a 135 degree laterally offset design (AltiVate system from DJO) All females with a lateralized implant had a 32 mm glenosphere with 6 mm of lateral COR offset, while all males had a 32 mm glenosphere with 10 mm of offset.
The reasons for choosing the different prostheses are not provided.
Lateralized prostheses were associated with higher LSAs (88 ± 7) vs. 82 ± 7 for medialized prostheses. While the difference was statistically significant, there was substantial overlap.
The distalization shoulder angle did not correlate with humeral lengthening.
Neither the DSA or the LSA were strongly correlated with 2-year postoperative American Shoulder and Elbow Surgeons score or shoulder range of motion.
Comment: This study did not include a multivariate analysis of the many demographic (e.g. age, sex, diagnosis) and surgical variables (e.g. implant type, size and position) that may influence outcome. On univariate analysis the authors did not find evidence to support the view that measurements of LSA and DSA have a major influence on the function of a reverse total shoulder.
Further study, probably using different measurements will be necessary to elucidate the reverse total shoulder geometries that are associated with the best function and the lowest risk of complications.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Shoulder arthritis - what you need to know (see this link) Shoulder arthritis - x-ray appearance (see this link) The smooth and move for irreparable cuff tears (see this link) The total shoulder arthroplasty (see this link). The ream and run technique is shown in this link. The cuff tear arthropathy arthroplasty (see this link). The reverse total shoulder arthroplasty (see this link).
Shoulder rehabilitation exercises (see this link).
This is a non-commercial site, the purpose of which is education, consistent with "Fair Use" as defined in Title 17 of the U.S. Code.
Note that author has no financial relationships with any orthopaedic companies.