These authors used finite element models of 3 arthritic scapulae with varying severities of posterior glenoid wear to compare 4 different implant configurations: standard glenoid implant in neutral alignment with asymmetric reaming, standard glenoid implant in retroversion, glenoid implant augmented with a posterior wedge in neutral alignment, and glenoid implant augmented with a posterior step in neutral alignment.
Contact between the humeral and glenoid components was simulated, and a compressive force of 625 N (representing 85% body weight) was applied through the humeral head into the glenoid surface.
They found that asymmetric reaming for the standard implant in neutral version required the most bone removal, resulted in the lowest percentage of back surface supported by cortical bone, and generated strain levels that risked damage to the most bone volume. In comparison to an asymmetric reaming for the standard implant in neutral version, a wedged implant removed less bone or insertion of a standard component in retroversion, had a significantly greater percentage of the back surface supported by cortical bone, and generated strain levels that risked damage to significantly less bone volume.
The results below compare the authors' wedge component (left), with a standard component inserted in retroversion (Std-R), with a stepped glenoid (Step) and a standard glenoid inserted after version 'correction'.
They concluded that the percentage of the back surface of the glenoid supported by cortical bone was associated with durability of the cement mantle; preservation of cortical bone may have the advantage of maintaining the structural integrity of cement mantle.
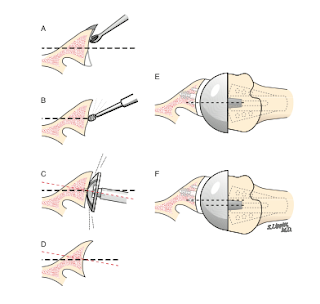
Comment: Like the authors, we are concerned about preserving glenoid cortical bone and about the amount of bone that can be sacrificed with the insertion of posteriorly augmented glenoid components as diagrammed below. If such a component were to fail, there would be a substantial bone defect.
If a glenoid component is elected this is inserted in a position of retroversion (below left), preserving bone in contrast to approaches that sacrifice bone to 'correct' retroversion (below right). The humerus is centered in the glenoid by soft tissue balancing and an eccentric humeral head component if necessary.
We have found that 'correction' of glenoid version is not necessary for the restoration of posterior stability and thus will ream the glenoid only as necessary to achieve a single concavity as shown below. So rather that using a guide pin inserted at a certain angle, we use a reamer that permits adjustment of the angle of reaming.
If a glenoid component is elected this is inserted in a position of retroversion (below left), preserving bone in contrast to approaches that sacrifice bone to 'correct' retroversion (below right). The humerus is centered in the glenoid by soft tissue balancing and an eccentric humeral head component if necessary.
As an example demonstrating that correction of glenoid version is not necessary, here's the case of a very active lady in her 60's with glenoid dysplasia.
Because of her activity level and glenoid retroversion of over 50 degrees we managed her shoulder with a ream and run procedure (one year post surgery films below).
She is back to kayaking and skiing without concern for polyethylene failure.
===
Check out the new Shoulder Arthritis Book - click here.
Use the "Search" box to the right to find other topics of interest to you.
You may be interested in some of our most visited web pages including:shoulder arthritis, total shoulder, ream and run, reverse total shoulder, CTA arthroplasty, and rotator cuff surgery as well as the 'ream and run essentials'