Instability and dislocation are major complications of reverse total shoulder arthroplasty (RSA) and are not easily solved by revision.
To help understand reverse shoulder stability and instability I will use some diagrams by Steve Lippitt from the 5th Edition of Rockwood and Matsens' The Shoulder (note that the completely revised 7th edition will be published next year - wait for it!). Steve was also critical to the understanding of concavity compression and describing the stability ratio (which will be discussed later in this post). See Glenohumeral stability from concavity-compression: A quantitative analysis
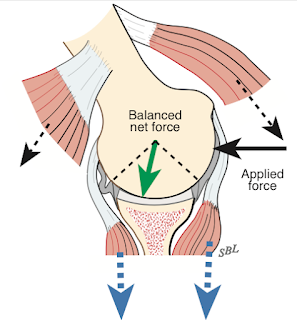
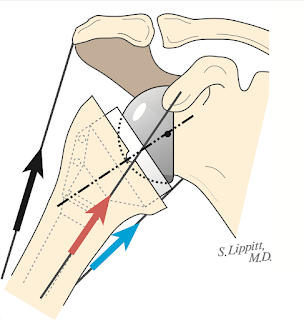
The reverse total shoulder is stabilized by conconcavity compression in which the concavity of the humeral polyethylene is pressed onto the glenosphere by the vector sum of muscle action, gravity and other forces (red arrow).
Dislocation can result when the compressive forces or the concavity of the humeral cup are insufficient to manage a displacing load, such as that from pushing one's self up from an armchair.I'll pick up the story from 2024 to the time of this writing (April 2025).
*Dislocation of the reverse total shoulder continues to be a major and prevalent issue for patients and surgeons
Mitigating the Risk of Instability After Reverse Shoulder Arthroplasty: A Critical Analysis Review of Patient and Surgical Factors Instability and dislocation after reverse shoulder arthroplasty may occur in up to 31% of patients. Clinical risk factors for instability include younger age, male sex, increased body mass index, preoperative diagnosis of proximal humerus fracture or rotator cuff pathology, history of instability of the native shoulder or after surgery, and a medical history of Parkinson's disease. In patients at a high risk of instability, surgeons should consider a more lateralized prosthesis (particularly in patients with an incompetent rotator cuff), repairing the subscapularis (particularly when using a medialized prosthesis), and upsizing the glenosphere (>40 mm in male and 38-40 mm in female patients). While potentially useful, less evidence exists for the use of a constrained liner.
Midterm outcomes of primary reverse shoulder arthroplasty: a systematic review of studies with minimum 5-year follow-up The rate of shoulder dislocation was 3.7% (0%-20.4%),
Instability after reverse shoulder arthroplasty: a retrospective review of thirty one cases The most frequent etiology for RSA instability was loss of compression, followed by impingement and loss containment.
Revision of reverse total shoulder arthroplasty: A scoping review of indications for revision, and revision outcomes, complications, and re-revisions 22% of the complications were dislocations or instability. 30% of the revisions were for dislocation or instability.
Predictors of dislocations after reverse shoulder arthroplasty: a study by the ASES complications of RSA multicenter research group. Patients with a primary diagnosis of glenohumeral osteoarthritis with an intact rotator cuff had an overall lower rate of dislocation than patients with other diagnoses (0.8% vs. 2.5%. Patient-related factors independently predictive of dislocation, in order of the magnitude of effect, were a history of postoperative subluxations before radiographically confirmed dislocation (odds ratio [OR]: 19.52), primary diagnosis of fracture nonunion (OR: 6.53), revision arthroplasty (OR: 5.61), primary diagnosis of rotator cuff disease (OR: 2.64), male sex (OR: 2.21), and no subscapularis repair at surgery (OR: 1.95).
Complications following reverse total shoulder arthroplasty for proximal humeral fractures: a systematic review The most common postoperative complication was prosthetic instability/dislocation: 2.3%
Complications after reverse shoulder arthroplasty for proximal humerus nonunion The most common postoperative complication was prosthetic instability/dislocation: 12%
Poor clinical outcomes and high rates of dislocation after modular reverse shoulder arthroplasty for proximal humeral oncologic resection Dislocations occurred in 40%
Intraoperative repair of functional subscapularis during RSA by deltopectoral approach could improve internal rotation but does not prevent anterior dislocation. In the functional repair group, three shoulders (1.2%) reported subjective instability and 1 (0.4%) dislocated.None occurred in in either the non-functional repair or non-repair groups.
Reverse shoulder arthroplasty with a 155 degrees neck-shaft angle inlay implant design without reattachment of the subscapularis tendon results in satisfactory functional internal rotation and no instability: a cohort study. One out of 210 prostheses was revised for dislocation within the first month after primary surgery.
Impact of morbid obesity on postoperative outcomes in reverse total shoulder arthroplasty: A national inpatient sample analysis Morbid obesity (BMI >/=40 kg/m(2)) was associated with a periprosthetic dislocation rate of 2.60 % in comparison to 1.59 % in controls
Impact of accumulating risk factors on the incidence of dislocation after primary reverse total shoulder arthroplasty using a medial glenoid-lateral humerus onlay prosthesis. 1.4% of the patients experienced dislocation with a medialized glenoid-lateralized humerus onlay rTSA prosthesis. The greatest risk factors for dislocation were male sex, age <68 years at the time of surgery, patients with body mass index >30, patients who received glenospheres having a diameter >40 mm, and patients who received expanded or laterally offset glenospheres.
Low success rate of closed reductions when treating dislocations after reverse shoulder arthroplasty: a study by the ASES Complications of RSA Multicenter Research Group. a closed reduction was initially attempted in the majority of patients, but only about one-third were successful and required no further intervention. Unsuccessful closed reductions were associated with higher patient BMI. Revision surgery for dislocations was complicated by a high rate of recurrent dislocations and rerevision surgery.
*The diameter, depth and orientation of the humeral cup affect stability of the reverse total shoulder. However, it must be remembered that the ability of the RSA to resist dislocation depends not only on the shape and orientation of the cup, but also on the direction and magnitude of the net force as shown by the red arrows in the first two diagrams at the start of this post.
.
Illustration of a reverse total shoulder arthroplasty: radius (r) of the glenosphere and concavity depth (d) or jump height of the liner are required to calculate the liner stability ratio (LSR). Yellow area: the extent of the glenosphere covered by the liner; yellow striped line: angle of coverage (degree of glenosphere coverage by the liner).
Patients having receiving RSA had an 8% dislocation rate for standard liners and a 0% dislocation rate for retentive liners. The authors attribute this difference to the jump height for the 36 mm standard implant of 8.1 and a linear stability ratio (LSR) of 152%; whereas the 36 mm retentive liner had a jump height of 10.1 and linear stability ratio of 195 to 202%
For this design, the most stable liner type was the 36 retentive:
They also found that the mean effective neck-shaft angle was 133 degrees (127-144 degrees) for short stems and 135 degrees (129-143 degrees) for long stems. Long stems significantly reduced varus outliers
Varus-valgus alignment of humeral short stem in reverse total shoulder arthroplasty: does it really matter? The utilization of short humeral stems in reverse total shoulder arthroplasty has gained attention, however, concerns exist regarding the risk of misalignment with implant insertion. In this cadaver study, anterior dislocation forces were considerably lower in the varus group compared to the neutral group. Valgus positioning did not significantly impact instability compared to the neutral position.
*Know the implants you're using
Large variability in degree of constraint of reverse total shoulder arthroplasty liners between different implant systems There were variations in jump height between rTSA systems at a given size, resulting in large differences in stability ratio. Standard liners exhibited a stability ratio range from 126% to 214% (mean 158% (SD 23%)) and constrained liners a range from 151% to 479% (mean 245% (SD 76%)). The angle of coverage showed a range from 103 degrees to 130 degrees (mean 115 degrees (SD 7 degrees) for standard liners and a range from 113 degrees to 156 degrees (mean 133 degrees (SD 11 degrees )) for constrained liners.
Four arthroplasty systems had constant stability ratios for standard liners (within 5%) across different sizes, while one system showed slight inconsistencies (within 10%), and ten arthroplasty systems showed large inconsistencies (range 11% to 28%). The stability ratio of constrained liners was consistent across different sizes in two arthroplasty systems and inconsistent in seven systems (range 18% to 106%).
Impact of constrained humeral liner on impingement-free range of motion and impingement type in reverse shoulder arthroplasty using a computer simulation The humeral liner may be changed to a constrained type when stability does not improve by increasing glenosphere size or lateralization with implants, and patients, particularly women with obesity, have risks of periprosthetic instability that may be secondary to hinge adduction on the thorax. This RSA computer simulation model demonstrated that constrained humeral liners led to decreased impingement-free ROM.
From Dr Stefan Bauer I received the most interesting response below.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link)
Shoulder rehabilitation exercises (see this link).