These authors state that failure of rotator cuff rotator cuff repair is common and a major cause of postoperative pain. "Retear rates are approximated at 7% to 17% for small tears and up to 41% to 94% for large and massive tears."
These authors retrospectively analyzed the data of 39 patients with shoulder pain after arthroscopic rotator cuff repair who had subsequently undergone shoulder sonography, followed by revision arthroscopy.
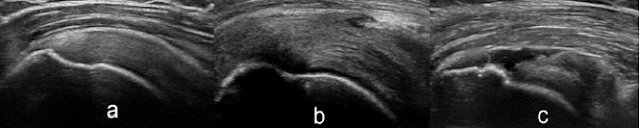
Sonography was performed by a single experienced shoulder surgeon, who has performed an average of 30 shoulder sonographic examinations per week for more than 20 years. A Sonosite 180 linear 3- to 11-MHz transducer was used with the depth adjusted to accommodate for differences in soft-tissue mass among the patients with ranges between 3 and 5 cm.
A rotator cuff retear was found on sonography 21 patients (54%) and on revision arthroscopy in 26 patients (67%). Sonography showed a sensitivity of 80.8% and specificity of 100% in the diagnosis of rotator cuff retears. If partial rehears were excluded, the sensitivity was 94.7%, and the specificity was 100%.
Comment: Since our original report in 1988 (Sonography of the Postoperative Shoulder (see this link), sonography has been used as cost-effective method for assessing shoulders for failure of rotator cuff repairs.
This study compares sonography to the gold standard of arthroscopic inspection, rather than to MRI.
MRI has been shown to have 84% sensitivity and 87% specificity in detecting recurrent rotator cuff tears in one study and 91% sensitivity and 25% specificity in detecting recurrent tears in another.
In assessing the outcomes of the large number of rotator cuff repairs that are carried out each year, it is essential that imaging of the repair at followup be carried out both in those patients who are improved and those who are not so that we can determine the role cuff integrity plays in the outcome.
=====
The reader may also be interested in these posts:
Consultation for those who live a distance away from Seattle.
Click here to see the new Shoulder Arthritis Book.
Click here to see the new Rotator Cuff Book
Information about shoulder exercises can be found at this link.
Use the "Search" box to the right to find other topics of interest to you.
You may be interested in some of our most visited web pages including:shoulder arthritis, total shoulder, ream and run, reverse total shoulder, CTA arthroplasty, and rotator cuff surgery as well as the 'ream and run essentials'
See from which cities our patients come.
See the countries from which our readers come on this post.