Overview of the articles
Functional internal rotation after shoulder arthroplasty is important to the quality of the outcome realized by the patient.
Limitation of functional internal rotation is common after reverse total shoulder arthroplasty. This is especially the case for patients with cuff tear arthropathy, poor preoperative internal rotation, and high body mass index.
Functional internal rotation is better for patients having anatomic total shoulder arthroplasty in comparison to those having reverse total shoulder arthroplasty
Functional internal rotation after reverse total shoulder arthroplasty is optimized by
Avoiding unwanted contact of the scapula with the humerus and humeral component
Lateralizing the glenoid center of rotation
Mildly inferiorly offsetting the glenosphere
Avoiding a constrained liner
Successfully repairing the subscapularis
Anatomically restoring the lateral humeral offset and humeral retroversion
Functional internal rotation is not associated with
Lateralization or distalization shoulder angles
Glenoid retroversion
Here are the articles
Understanding loss of internal rotation after reverse shoulder arthroplasty: a narrative review of current literature Functional internal rotation after RSA is optimized by maximizing impingement-free arc of motion and subscapularis repair in patients with mobile scapulothoracic joints, adequate preoperative humerothoracic extension, and low body mass index.
Do internal rotation and global range of motion affect patient outcomes?
Internal rotation limitation is prevalent following modern reverse shoulder arthroplasty and negatively affects patients' subjective rating of the procedure 59% of patients having RSA reported subjective internal rotation (IR) limitations, and 41% had objective IR limitations. Comparison of preoperative and postoperative IR showed that 24% had worsened IR, whereas 33% improved. Limited IR was associated with lower patients' subjective rating of RSA and negatively affected PROMs. Regression analysis showed that limited IR was the only independent determining factor that was significantly associated with a lower subjective rating of RSA. "Despite advancements in RSA design, limited IR remains a prevalent issue, significantly affecting patients' satisfaction and clinical outcomes."
Restoration of internal rotation after reverse shoulder arthroplasty may vary depending on etiology in patients younger than 60 years of age: a multicenter retrospective study "The restoration of active internal rotation with the elbow at the side remains the main functional weak link of RSA" Patients with easy active internal rotation had better Constant scores, as well as improved motion in forward elevation.
Is There an Association Between Postoperative Internal Rotation and Patient-reported Outcomes After Total Shoulder Arthroplasty? An acceptable outcome (SANE score of > 75%) was associated with sufficient internal rotation reach to the midback or higher.
Thresholds for diminishing returns in postoperative range of motion after total shoulder arthroplasty Postoperative range of motion (ROM) of more than 113 degrees of abduction, 162 degrees of FE, 52 degrees of ER, and IR to L1 added only minimal \ improvement in the Simple Shoulder Test, American Shoulder and Elbow Surgeons score, and the Shoulder Pain and Disability Index.
How do reverse and anatomic total shoulders compare with respect to range of motion?
Evaluation of New Normal After Shoulder Arthroplasty: Comparison of Anatomic versus Reverse Total Shoulder Arthroplasty In comparison to 40% of patients having anatomic total shoulder arthroplasty (aTSA) only 26% of reverse total shoulder arthroplasty (rTSA) patients (rTSA) reached a SANE score > 95 (100 = "normal" function). aTSA significantly outperformed rTSA in American Shoulder and Elbow Surgeons (ASES) score, ability to reach a high shelf, lift 10 pounds, perform usual work and perform usual sport, Simple Shoulder Test (SST) score, ability to lift 8 pounds and carry 20 pounds, range of motion including clinician measured elevation, abduction, external rotation, and internal rotation.
Comparison between Anatomic Total Shoulder Arthroplasty and Reverse Shoulder Arthroplasty for Older Adults with Osteoarthritis without Rotator Cuff Tears The aTSA group demonstrated significantly better postoperative ASES and Constant-Murley scores than the RSA group. The TSA group showed a significantly better postoperative active ROM than the RSA group regarding forward flexion as well as external and internal rotations. "Clinical results and ROM were better with TSA than with RSA during the short- and mid-term follow-up periods."
Comparison of Anterior Shoulder Pain and Internal Rotation Dysfunction after Anatomic and Reverse Shoulder Arthroplasty for Osteoarthritis used an anterior shoulder pain and dysfunction survey (ASPDS) to classify anterior shoulder dysfunction and used the functional internal rotation (FIR) score, to quantify internal rotation (IR) deficiency following RSA compared to aTSA when performed for osteoarthritis. ASPDS scores were lower in the RSA group compared to the aTSA group. Mean FIR scores was also worse in the RSA group compared to the aTSA group. "Findings suggest that anterior shoulder pain and dysfunction and decreased internal rotation are more common in RSA compared to aTSA when performed for osteoarthritis, with differences observed at two years postoperatively. These differences in outcomes were not captured by traditional shoulder outcomes questionnaires.
Exactech Equinoxe Anatomic Versus Reverse Total Shoulder Arthroplasty For Primary Osteoarthritis with an Intact Rotator Cuff in Patients with No Glenoid Deformity aTSAs had more favorable abduction, internal rotation, external rotation, Constant score, and SAS score.
What are the factors that affect internal rotation after a reverse total shoulder?
Preoperative diagnosis and rotator cuff status impact functional internal rotation following reverse shoulder arthroplasty Patients who undergo RSA for primary osteoarthritis have a better chance of postoperative improvement in functional internal rotation (fIR). A decrease in fIR is common after RSA for massive irreparable cuff tears.
Predictive factors influencing internal rotation following reverse total shoulder arthroplasty. Poor preoperative functional IR was risk factor for poor postoperative IR. BMI was inversely correlated with degree of IR after RTSA. Preoperative opioid use was found to negatively affect IR. Glenoid retroversion, glenoid lateralization, and individualized component positioning affected postoperative IR.
Influence of preoperative rotational shoulder stiffness on rate of motion restoration after anatomic and reverse total shoulder arthroplasty for glenohumeral osteoarthritis with an intact rotator cuff Preoperative stiffness is associated with slower recovery of active ROM over a longer duration in patients undergoing shoulder arthroplasty for RCI-GHOA.
Varus-valgus alignment of humeral short stem in reverse total shoulder arthroplasty: does it really matter? The varus position enhances rotational range of motion (ROM) but increases instability, while the valgus position does not significantly impact ROM or instability compared to the neutral position.
Humeral Component Version Has No Effect on Outcomes Following Reverse Total Shoulder Arthroplasty: A Prospective, Double-Blinded, Randomized Controlled Trial Securing the humeral component at neutral version or 30 degrees of retroversion in rTSA resulted in similar active shoulder external rotation, internal rotation, forward elevation, abduction, and strength measurements, complication rates, and VAS pain, PROMIS-10 physical, and ASES scores at 2 years postoperatively
Analysis of three different reverse shoulder arthroplasty designs for cuff tear arthropathy - the combination of lateralization and distalization provides best mobility CTA patients with a lateralized and distalized RSA configuration were associated with achieving better flexion and abduction with less scapular notching. A better rotation was associated with either of the lateralized RSA designs in comparison with the classic Grammont prosthesis.
Glenoid lateralization and subscapularis repair are independent predictive factors of improved internal rotation after reverse shoulder arthroplasty After Grammont-style RSA two surgical factors were associated with better AIR after RSA: glenoid lateralization (with BIO-RSA technique) and subscapularis repair. Internal rotation was functional (>/= L3 level) in 67% of operated shoulders.
Lateralization and distalization shoulder angles do not predict outcomes in reverse shoulder arthroplasty for cuff tear arthropathy There was no association between lateral shoulder angle (LSA) or distal shoulder angle (DSA) measurements and 2-year functional outcomes after RSA.
Modified distalization shoulder angle and lateralization shoulder angle show weakly correlation with clinical outcomes following reverse shoulder arthroplasty DSA and LSA show minimal correlation with postoperative outcomes and have limited predictive value.
Lateralization and Distalization Shoulder Angles in Reverse Shoulder Arthroplasty: Are They Still Reliable and Accurate in All Patients and for All Prosthetic Designs? While prosthetic design and preoperative shoulder anatomy have a significant influence on LSA and DSA measurements in RSA, optimal LSA and DSA values may lack validity and reliability.
Increased glenoid baseplate retroversion improves internal rotation following reverse shoulder arthroplasty With a 135 degree and lateralized glenoid, postoperative baseplate retroversion of >10 degrees was associated with significantly improved internal and external rotation at 90 degrees, Constant-Murley, and Single Assessment Numeric Evaluation scores at 2-year follow-up compared to <10 degrees retroversion. Additionally an increased change in version from preoperative to postoperative appears to improve internal rotation with the arm at 90 degrees without limiting external rotation in adduction or forward flexion. While baseplate retroversion does not improve internal rotation, overall function appears to be improved and therefore consideration may be given to accepting retroversion or intentionally retroverting the baseplate if fixation allows.
Baseplate inferior offset affects shoulder range of motion in reverse shoulder arthroplasty in Asian population The range of motion in abduction, flexion, and internal and external rotations significantly improved with increased inferior baseplate offset.
Baseplate version in reverse shoulder arthroplasty: does excessive retroversion or anteversion affect functional activities of daily living? High values of baseplate retroversion or anteversion were not associated with inferior patient reported outcomes or functional rotation after reverse total shoulder arthroplasty
Virtual assessment of internal rotation in reverse shoulder arthroplasty based on statistical shape models of scapular size. Glenosphere position required to maximize IR varied by scapula size. For smaller scapulae, maximum IR at 0 degrees (IR0) was reached with a combination of 2.5-mm inferior offset and 0-4 mm of lateralization. For larger scapulae, maximum IR0 was reached with a combination of 2.5 mm of inferior offset and 4 mm of lateralization. Maximum IR in 60 degrees of abduction was reached in smaller scapula with 4-6 mm of lateralization and at least 12 mm of lateralization in larger scapula.
Functional internal rotation is associated with subscapularis tendon healing and increased scapular tilt after Grammont style bony increased offset reverse shoulder arthroplasty with 155 degrees humeral implant This study revealed that in a Grammont-type RSA, postoperative internal rotation behind the back recovery is first associated with subscapularis tendon healing, followed by passive internal rotation at 90 degrees of abduction and finally the ability to tilt the scapula anteriorly.
Healed subscapularis and its clinical implications for internal rotation in humeral lateralized reverse shoulder arthroplasty Healed subscapularis (SSC) groups had significantly better IR aROM, and IR strength than both nonhealed and nonrepaired SSC groups.
Comparative Efficacy of Latissimus Dorsi and Teres Major Versus Pectoralis Major Tendon Transfers Combined with Exactech Equinoxe Reverse Total Shoulder Arthroplasty in Improving Internal Rotation: A Preliminary Result Both latissimus dorsi and teres major (LDTM) and pectoralis major (PM) transfers combined with RTSA significantly improve clinical outcomes in patients with massive cuff tears and cuff tear arthropathy who had a loss of active IR. The LDTM transfer is superior for IR aROM with the arm behind the back, while the PM transfer more effectively improves IR strength in front of body.
Avoiding unwanted contact.
Optimizing range of motion in reverse shoulder arthroplasty Lateralizing the glenoid component by using an angled bony or metallic augment of 8 to 10 mm provides optimal impingement-free ROM.
Impact of constrained humeral liner on impingement-free range of motion and impingement type in reverse shoulder arthroplasty using a computer simulation This RSA computer simulation model demonstrated that constrained humeral liners led to less impingement-free ROM. A lateralized glenosphere improved abduction ROM.
Reverse shoulder arthroplasty implant design and configuration has a significant effect on conjoint tendon impingement Conjoint tendon impingement can be associated with larger glenospheres, anterosuperior baseplate and glenosphere positioning, humeral implants or trays positioned medial and posterior, and increased humeral component retroversion.
Eccentricity and greater size of the glenosphere increase impingement-free range of motion in glenoid lateralized reverse shoulder arthroplasty: A computational study A greater glenoid size and eccentric glenoid type allowed for more mobility. A 135 degrees stem allowed greater mobility in all movements except for abduction than a 155 degree inlay stem.
Preoperative Planning and Inferior Glenosphere Overhang Increases the Odds of Achieving High Internal Rotation After Univers Reverse Total Shoulder Arthroplasty Specific baseline patient characteristics influence the ability to obtain high IR after rTSA including increased preoperative IR, BMI, and surgery on the dominant arm. There are several factors within the surgeon's control: inferior glenosphere overhang and slight distalization increased postoperative IR.
Preoperative Planning Software Does Not Accurately Predict Range of Motion in Reverse Total Shoulder Arthroplasty The passive glenohumeral impingement-free ROM generated from preoperative planning incompletely predicts clinically measured active humerothoracic ROM, possibly because of the unmeasured factors of soft-tissue tension, muscular strength, humeral torsion, resting scapular posture, and, most importantly, scapulothoracic motion.
Posteroinferior glenosphere positioning is associated with improved range of motion following reverse shoulder arthroplasty with a 135 degrees inlay humeral component and lateralized glenoid posteroinferior glenosphere position may improve ROM when using a 135 degrees inlay humeral component and a lateralized glenoid.
The case for an anatomic reconstruction
Development, Evolution, and Outcomes of More Anatomical Reverse Shoulder Arthroplasty The original Grammont-style RSA revolutionized shoulder arthroplasty but had several limitations, including scapular notching and reduced rotational motion. The development of a lateralized center of rotation construct aimed at addressing the limitations associated with the Grammont-style design and to more closely reproduce the native anatomy in order to improve patient outcomes.
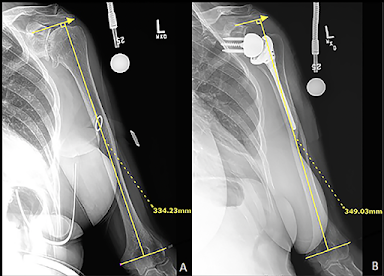
Anatomic restoration of lateral humeral offset and humeral retroversion optimizes functional outcomes following reverse total shoulder arthroplasty. Greater deviations from pre-op lateral humeral offset was predictive of poorer IR ROM. Patients with minimal deviations in humeral retroversion (post-op humeral retroversion (HR) within 10 degrees of pre-op HR) and minimal deviations in lateral humeral offset (LHO) (post-op LHO </= pre-op LHO) displayed the greatest postoperative ER ROM.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link)
Shoulder rehabilitation exercises (see this link).