His conclusions can be summarized as follows:
(1) baseplate failure is an import complication of reverse total shoulder arthroplasty
(2) time zero (immediate post op) stability of the baseplate is important because (a) the patient will load the baseplate before any bone ingrowth has had time to occur and (b) micro motion of the baseplate will inhibit bone ingrowth so that the screws may be all that is holding the baseplate to the glenoid bone leading to the risk of fatigue fracture
(3) failure to remove cartilage and interposed tissue between baseplate and bone may prevent adequate seating of the baseplate
(4) as is the case with all screw fixation in bone, bone quality has a strong effect on the quality of fixation: (a) low bone density may result in lack of a solid "bite" (screw stripping); (b) high bone density may result in incomplete seating
(5) from plain radiographs, the surgeon can preoperatively get an idea of the glenoid bone density: poor (below left), sclerotic (below right).
(6) for bone suspected of having poor bone quality, the author uses some straightforward innovations that do not add time, technology or expense:
(a) for soft bone the glenoid is reamed over a 2.5 mm drill (without using a tap) followed by insertion of the baseplate in the untapped bone
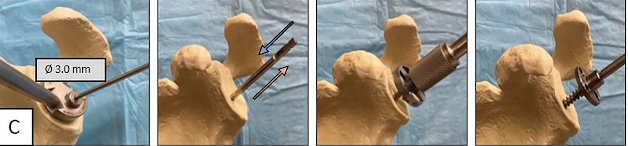
(b) for denser than average bone, a 3.0-mm drill is used for the pilot hole, and then the tap is passed (inserted and removed) a total of 3 times, followed by insertion of the baseplate in the tapped bone (c) the standard technique is used for average density bone: a 2.5-mm drill is inserted in the central hole to a depth of 30 mm, followed by use of the 6.5-mm tap, reaming of the glenoid, and finally, insertion of the monoblock baseplate
In in vitro testing using a low-density block model, the standard technique gave a compressive force of 112 N compared with 300 N for the soft bone technique.
In the high-density bone model, the standard technique resulted in failure to seat the baseplate, or screw breakage. Performing the dense bone technique, the baseplate was seated without failure, with an average compressive force of 450 N.
Comment: Time zero (initial) fixation is important for minimizing the risk of baseplate failure. This requires adequate bone preparation for maximal baseplate-bone contact, full seating of the baseplate and placement of the peripheral screws in good quality bone.
The inspection of preoperative plain radiographs and the use of the techniques suggested here can reduce the risk of inadequate compression on one hand and incomplete seating on the other.
It is noted that with this implant system, the only screw providing substantial compression is the central one - the others are locking screws.
Finally, in cases where the central screw is stripped, we have found that "match stick" strips of cortical bone can be progressively added to the central hole until good compression is achieved.
Comments welcome at shoulderarthritis@uw.edu
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).