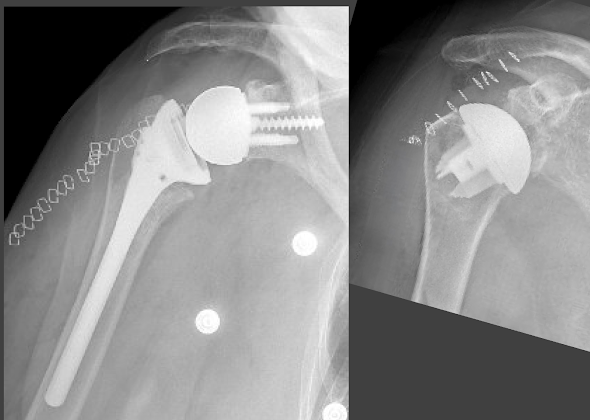
One of the most frequently debated topics in shoulder surgery is the choice between reverse total shoulder (RSA, below left) and anatomic total shoulder (aTSA below right) for patients having osteoarthritis with an intact rotator cuff.
This is going to be an upside down post. First the conclusions and then the published evidence from 2024-2025.
Conclusions
(1) Patients having either aTSA or RSA have good reported outcomes. While some papers have reported statistically significant benefits of one or the other, most of these differences are not clinically significant (i.e. the difference does not exceed the minimal clinically important difference (MCID)). However, there is evidence that shoulder internal and external rotation is better with aTSA and that rotation matters to the patient. The effect of rotation on patient function may not be noted on ASES, VAS, and SANE scores. In contrast three of the 12 Simple Shoulder Test questions relate to shoulder rotation: (3) Can you reach the small of your back to tuck in your shirt?, (4) Can you place your hand behind your head with your elbow straight out to the side? and (11) Can you wash the back of your opposite shoulder?
(2) The complications for the two procedures are different. For RSA, along with instability, intraoperative and postoperative fractures and infections loom large. These observations suggest the need for RSA techniques and implants that respect the often compromised bone quality coupled along with minimizing procedure time and optimizing infection prophylaxis. For aTSA, rotator cuff tears and glenoid component loosening top the list. This suggests the need for thoughtful patient selection with respect to cuff status and technical attention to achieving excellent glenoid component seating. It is worth noting that complication rate and revision rate are different, in that some complications (e.g. acromial/spine fractures) are often managed without revision.
(3) Preoperative stiffness and preoperative weakness are not strongly associated with bettter outcomes for RSA in comparison to aTSA.
(5) The revision rate for stemless aTSA may be comparable to that for RSA and lower than that for stemmed TSA. There is a suggestion that cuff failure may be less common in stemless aTSA in comparison to stemmed aTSA.
(6) The type of fellowship taken by the surgeon appears to influence the type of arthroplasty selected for osteoarthritis.
(7) The cost of RSA is greater than the cost of aTSA
Now here are the articles.
Is There an Association Between Postoperative Internal Rotation and Patient-reported Outcomes After Total Shoulder Arthroplasty? After shoulder arthroplasty, shoulder normalcy was associated with postoperative internal rotation
Comparison of Anterior Shoulder Pain and Internal Rotation Dysfunction after Anatomic and Reverse Shoulder Arthroplasty for Osteoarthritis Using a new anterior shoulder pain and dysfunction survey (ASPDS) the authors classified anterior shoulder dysfunction and use following RSA compared to aTSA when performed for osteoarthritis. At 2 years after surgery, mean ASPDS scores were worse in the RSA group compared to the aTSA group. Mean functional internal rotation scores were also worse in the RSA group compared to the aTSA group. Notably, no differences reaching statistical significance were observed between aTSA and RSA groups for ASES, SANE or VAS pain scores.
Internal rotation based activities of daily living show limitations following reverse shoulder arthroplasty versus anatomic shoulder arthroplasty PROMs were mostly similar between aTSA and rTSA, however the Simple shoulder test (SST) did show a difference with better scores in the aTSA cohort. The activities of daily living that showed significant disparity between aTSA and rTSA were toileting, donning a coat, reaching one’s back as well as throwing overhand with rTSA patients reporting more difficulty in all these ADLs after RSA.
A comparative analysis of anatomic total shoulder arthroplasty versus reverse shoulder arthroplasty for posterior glenoid wear patterns considered patients with B2 and B3 glenoid types. At two year followup, TSA patients had better average active external rotation and internal rotation. There was no significant difference in complication rate. The most common complication was cephalic vein thrombosis. No complication required revision.
Patients undergoing reverse total shoulder arthroplasty have less pain and require fewer opioid pain medications compared to anatomic total shoulder arthroplasty in the early postoperative period: a retrospective review found that while aTSA patients required more opioid medication refills and remained on opioids for a longer duration in the early postoperative period, by 12 weeks there was no difference in the VAS pain score or the percent of patients taking opioids. As shown below, aTSA patients had significantly better rotation than RSA patients at 12 weeks.


Improvement in Sleep Disturbance Following Anatomic and Reverse Shoulder Arthroplasty The ability to sleep comfortably returned faster than the ability to sleep on the affected side, with the ability to sleep comfortably reaching a plateau at 3 months and the ability to sleep on the affected side reaching a plateau at 6 months. 13.2% of patients in the TSA group and 16.0% of those in the RSA group could not sleep comfortably and 31.4% of those in the TSA group and 36.8% of those in the RSA group could not sleep on the operative side.
Reverse versus anatomic total shoulder arthroplasty for glenohumeral osteoarthritis with intact cuff: a meta-analysis of clinical outcomes found no clinically significant differences in patient reported outcomes. The aTSA group had a significantly more external rotation relative to the RSA group. Twelve studies reported adverse outcomes, with the RSA group having a lower rate of complications and reoperations relative to aTSA at an average follow-up of 3.4 years.

Total Shoulder Arthroplasty Versus Reverse Shoulder Arthroplasty in Primary Glenohumeral Osteoarthritis With Intact Rotator Cuffs: A Meta-Analyses found no significant differences in forward elevation, external rotation in adduction, internal rotation, visual analog scale (VAS), American Shoulder and Elbow Surgeons (ASES) score, and Single Assessment Numeric Evaluation (SANE) scores. There were a total of 20 (3.68%) complications in the aTSA group and eight (2.4%) complications in the RSA group. The complications in the aTSA group consisted of seven radiographic failures, six subscapularis failures, three posterior dislocations, two late rotator cuff insufficiencies, one arthrofibrosis, and one wound infection. The complications in the RSA group consisted of four acromial stress fractures, two baseplate fractures, one periprosthetic infection, and one periprosthetic fracture.
Comparison between Anatomic Total Shoulder Arthroplasty and Reverse Shoulder Arthroplasty for Older Adults with Osteoarthritis without Rotator Cuff Tears found that the TSA group demonstrated significantly better postoperative ASES and Constant-Murley scores than the RSA group, but these differences did not exceed the MCID for these measures. The TSA group showed a significantly better postoperative active ROM than the RSA group regarding forward flexion as well as external and internal rotations.
Anatomic and Reverse Total Shoulder Arthroplasty for Osteoarthritis: Outcomes in Patients 80 Years Old and Older At most recent follow-up, there were no significant differences in PROMs between cohorts. aTSA patients achieved greater postoperative motion in external rotation and internal rotation. There were six complications amongst aTSA patients (7.8%): four with subscapularis insufficiency, one humeral shaft periprosthetic fracture treated with open reduction and internal fixation, and one with prosthetic joint infection revised to a functional composite spacer. Three rTSA patients (5.6%) sustained complications – all acromion/scapular spine fractures (2 Type 2; 1 Type 3) which were treated non-operatively.
Reverse total shoulder arthroplasty for primary osteoarthritis with restricted preoperative forward elevation demonstrates similar outcomes but faster range of motion recovery compared to anatomic total shoulder arthroplasty Postoperative active flexion and external rotation were similar between RSA and TSA cohorts. Internal rotation was worse in the RSA cohort. RSA led to faster postoperative FF and ER recovery. There was no statistically significant difference in complication rates between cohorts.
Clinical outcomes of anatomic vs. reverse total shoulder arthroplasty in primary osteoarthritis with preoperative external rotation weakness and an intact rotator cuff: a case-control study In preoperatively weak patients with cuff-intact primary osteoarthritis, aTSA leads to similar postoperative strength, range of motion, and outcome scores compared with patients with normal preoperative strength, indicating that preoperative weakness does not preclude aTSA use. Patients who were preoperatively weak in ER demonstrated improved postoperative rotational motion after undergoing aTSA and rTSA, with both groups achieving the minimal clinically important difference and substantial clinical benefit at similar rates.
Does preoperative forward elevation weakness affect clinical outcomes in anatomic or reverse total shoulder arthroplasty patients with glenohumeral osteoarthritis and intact rotator cuff? Patients with cuff intact glenohumeral arthritis and preoperative FE weakness obtain postoperative outcomes similar to patients with normal preoperative strength after either aTSA or rTSA. Preoperatively weak aTSAs achieved greater ER but lower rates of clinically relevant improvement in overhead motion compared to weak rTSAs.
Anatomic Versus Reverse Total Shoulder Arthroplasty for Primary Osteoarthritis With an Intact Rotator Cuff: A Midterm Comparison of Early Top Performers Active external rotation (ER) was greater after aTSA at midterm follow-up in both ASES and SAS score cohorts; however, preoperative to postoperative improvement was equivalent. Postoperative ER and SAS scores were greater after aTSA. No difference was found in the incidence of complications and revision surgeries between top-performing aTSAs and rTSAs.
Treatment of B2 Type Glenoids with Anatomic versus Reverse Total Shoulder Arthroplasty: A Retrospective Review Postoperatively patients in the aTSA group had significantly better external rotation and internal rotation compared to the rTSA group. There were no differences in patient reported outcomes between the two groups. No patients in the aTSA group had recurrent posterior humeral head subluxation. Eight complications requiring revision occurred, 4 in each group.
The authors of Stemless anatomic and reverse shoulder arthroplasty in patients under 55 years of age with primary glenohumeral osteoarthritis: an analysis of the Australian Orthopedic Association National Joint Replacement Registry at 5 years stated that instability was the predominant cause of revision for reverse total shoulder arthroplasty (rTSA), and stemmed aTSA, while loosening was the predominant cause of revision for stemless aTSA (SLaTSA). The 6-year cumulative percent revision rate was 12.4% for stemmed aTSA (instability, loosening, cuff failure, infection), 7.0% for SLaTSA (instability, loosening, infection) and 6.5% for rTSA (instability, infection) .
Anatomic or reverse total shoulder arthroplasty? How fellowship training affects selection of arthroplasty type Surgeons having completed a Sports Medicine fellowship chose rTSA over ATSA at a higher rate than those who completed a shoulder and elbow fellowship, both for all indications and for a primary diagnosis of glenohumeral osteoarthritis.
Trends in Total Shoulder Arthroplasty Utilization and Implant Pricing from 2017 to 2022 the inflation-adjusted cost of aTSA decreased from $8055 in 2013 to $6223 in 2022, and RSA from $12,207 to $8882 in 2022
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link)
Shoulder rehabilitation exercises (see this link).
