The authors of Successful Management of Periprosthetic Joint Infection Following Total Joint Arthroplasty, as Defined by the Patient have noted that the literature on the subjective experience of patients undergoing treatment for periprosthetic joint infection (PJI) following total joint arthroplasty (TJA) is scarce, and treatment success is defined without consideration of patient values.
They undertook a study to characterize the experience of 27 patients undergoing PJI management, to identify factors that patients associate with successful treatment and to assess alignment with a 2019 outcome-reporting tool (ORT) by the Musculoskeletal Infection Society (MSIS). Included patients had 1 to 5 year followup after their most recent revision surgery.
Patients participated in interviews that documented their experiences with primary TJA, PJI diagnosis and management, and patient perceptions of the success of their PJI management.
21 (78%) reported considerable mental health impacts during the period from PJI onset to treatment conclusion. In defining successful PJI management, patients consistently emphasized the importance of function, pain relief, mobility, and independence. Nine (33%) of the patients did not agree with their MSIS ORT classification of success versus failure.
Patients endorsed feelings of invalidation and a delay to diagnosis during PJI onset. They described a lack of understanding and preparedness for PJI, which contributed to negative emotions such as sadness, anger, and surprise at the time of PJI diagnosis. During the operative course and rehabilitation, patients struggled with physical limitations; this was especially noted among patients who underwent 2-stage revision. A common theme was the negative impact on patient mental health.
And the decision to use a single or two stage revision, recognizing the potential downsides of a spacer.
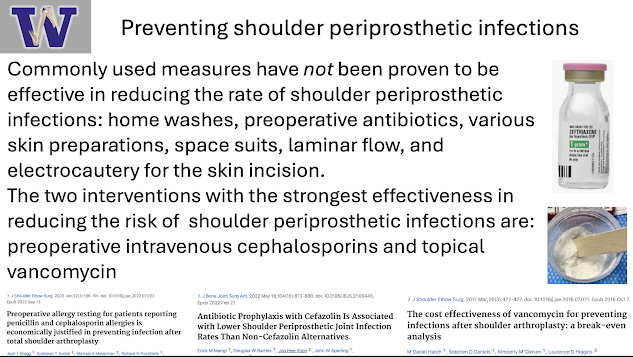
All of this is to support reasonable efforts to minimize the risk of PJI including optimization of health and nutrition, smoking cessation, and avoiding recent cortisone injections as stressed in this post and to consider the information in the slide below from a recent presentation on the topic.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link)
Shoulder rehabilitation exercises (see this link).