Degenerative joint disease is also known as osteoarthritis, osteoarthrosis or wear and tear arthritis. The pathogenesis of this condition results from the age-related loss of the ability of articular cartilage to sustain itself against seemingly minor mechanical imbalances and years of use. Degenerative joint disease typically affects healthy and active individuals. In our practice, most patients with degenerative glenohumeral degenerative joint disease are of Northern European ancestry in contrast to those of Asian, Southern European, Hispanic and African ancestry. In degenerative joint disease the glenoid cartilage and subchondral bone are progressively lost - either concentrically medially (more characteristic of female shoulders and those with inflammatory arthritis) or eccentrically posteriorly, with the articular cartilage often left intact anteriorly (more characteristic of male shoulders and those with degenerative joint disease or capsulorrhaphy arthropathy). The concern with the eccentric wear pattern is that the diminished articular contact area results in increased force/unit area leading to increased posterior wear which in turn leads to even less contact area. The cartilage of the humeral head is eroded in a Friar Tuck pattern of central baldness, often surrounded by a rim of remaining cartilage and osteophytes
The bone underlying the joint surfaces is usually sclerotic, but degenerative cysts can occur in the humeral head or glenoid; when severe, glenoid cysts may jeopardize the fixation of prosthetic glenoid components
In its early stages, degenerative glenohumeral joint disease may be only visible on the ‘truth view’
Later on, osteophytes typically surround the anterior, inferior, and posterior aspects of the humeral head and the inferior and posterior glenoid. As a result, the humeral and glenoid articular surfaces may take on a flattened configuration that blocks rotation
We have named the commonly seen inferior humeral osteophyte the ‘goat’s beard’
Loose bodies are often found in the axillary or subscapularis recesses. The pathoanatomy of the arthritic glenoid may include medial erosion, posterior erosion, and retroversion along with varying degrees of posterior humeral subluxation. The triad of glenoid biconcavity, glenoid retroversion, and posterior humeral subluxation – the ‘bad arthritic triad’ - is commonly found in primary degenerative joint disease. Progressive contracture of the anterior capsule limits external rotation and compounds the tendency of the humeral head to translate posteriorly. Major biceps pathology and substantial rotator cuff defects are uncommon in patients with primary degenerative joint disease. The common clinical course is one of slowly progressive loss of the ability to sleep and to use the shoulder for work and recreation because of shoulder pain and stiffness.
It is of note that young individuals are less likely to have primary glenohumeral osteoarthritis and more likely to have capsulorrhaphy arthropathy, secondary degenerative joint disease or other more complex forms of arthritis, many of which are the result of injury, prior surgery, or systemic disease. This, along with their increased longevity and increased activity expectations, may help explain the diminished satisfaction and increased rate of arthroplasty complications for younger individuals after shoulder arthroplasty. A number of these important but less straightforward diagnoses are discussed below.
Secondary Degenerative Joint Disease
In contrast to primary degenerative joint disease - that arises without a specific cause - secondary degenerative joint disease develops when previous injury or surgery affects the joint surface and precipitates its degeneration. The presentation and clinical course of each case depend on the underlying etiology of the secondary arthritis.
Anchor arthropathy is a type of secondary degenerative joint disease in which the glenohumeral joint surfaces are destroyed by prominent suture anchors used for repair of SLAP lesions
It is of note that young individuals are less likely to have primary glenohumeral osteoarthritis and more likely to have capsulorrhaphy arthropathy, secondary degenerative joint disease or other more complex forms of arthritis, many of which are the result of injury, prior surgery, or systemic disease. This, along with their increased longevity and increased activity expectations, may help explain the diminished satisfaction and increased rate of arthroplasty complications for younger individuals after shoulder arthroplasty. A number of these important but less straightforward diagnoses are discussed below.
Secondary Degenerative Joint Disease
In contrast to primary degenerative joint disease - that arises without a specific cause - secondary degenerative joint disease develops when previous injury or surgery affects the joint surface and precipitates its degeneration. The presentation and clinical course of each case depend on the underlying etiology of the secondary arthritis.
Anchor arthropathy is a type of secondary degenerative joint disease in which the glenohumeral joint surfaces are destroyed by prominent suture anchors used for repair of SLAP lesions
or for Bankart repairs
In this situation the suture anchors excoriate the humeral joint surface, which then erodes the glenoid surface. In cases of anchor arthropathy – or indeed any prior glenohumeral surgery - it is important to be alert to the possibility of infection with Propionibacterium
Post-traumatic arthropathy
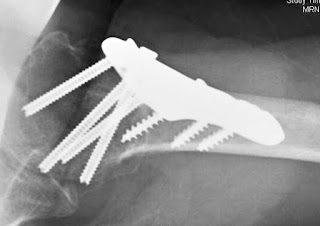
This is a condition in which prior injury has damaged the joint surfaces or given rise to malunion with joint incongruity, instability, non-unions and/or post-traumatic avascular necrosis without or with problems related to fixation hardware
Anterior or posterior dislocations may be followed by dislocation arthropathy. In unreduced dislocations, the humeral head may be indented and worn
The cartilage of the joint surfaces may be replaced by scar tissue, or the subchondral bone may be so weakened by bone atrophy that it collapses after reduction, resulting in an incongruous joint surface.
Shoulders with secondary degenerative joint disease often have complex pathology that challenges surgical management., Each case presents its own particular combination of capsular contracture, scarring, malunion, nonunion, bone loss, bone fragility, non-anatomic location of neurovascular structures and the presence of hardware from prior procedures.
Capsulorrhaphy Arthropathy
Capsulorrhaphy arthropathy is the name we have given to a special type of secondary degenerative joint disease in which deterioration of the joint surface is related to a previous repair for recurrent dislocations. It is one of the most common causes of severe arthritis in persons younger than 55 years. Capsulorrhaphy arthropathy may be caused by over tightening the anterior capsule; when external rotation is limited by a Putti–Platt repair, a Bankart repair or a Bristow/Latarjet procedure. Obligate posterior translation can force the humeral head out of its normal concentric relationship with the glenoid fossa. The posterior glenoid is typically eroded from this chronic posterior humeral subluxation, and major posterior bone deficiencies can result.
Shoulders with secondary degenerative joint disease often have complex pathology that challenges surgical management., Each case presents its own particular combination of capsular contracture, scarring, malunion, nonunion, bone loss, bone fragility, non-anatomic location of neurovascular structures and the presence of hardware from prior procedures.
Capsulorrhaphy Arthropathy
Capsulorrhaphy arthropathy is the name we have given to a special type of secondary degenerative joint disease in which deterioration of the joint surface is related to a previous repair for recurrent dislocations. It is one of the most common causes of severe arthritis in persons younger than 55 years. Capsulorrhaphy arthropathy may be caused by over tightening the anterior capsule; when external rotation is limited by a Putti–Platt repair, a Bankart repair or a Bristow/Latarjet procedure. Obligate posterior translation can force the humeral head out of its normal concentric relationship with the glenoid fossa. The posterior glenoid is typically eroded from this chronic posterior humeral subluxation, and major posterior bone deficiencies can result.
Shoulder arthroplasty for capsulorrhaphy arthropathy is associated with high rates of revision surgery and unsatisfactory outcomes because of instability, subscapularis failure, glenoid component failure after total shoulder arthroplasty, and pain from glenoid arthrosis after hemiarthroplasty. The importance of these poor results is heighted by the young age of the individuals commonly affected.
Rheumatoid and Other Types of Inflammatory Arthritis
Rheumatoid arthritis is a systemic disease with highly variable clinical manifestations. It can appear to be isolated to the glenohumeral joints or can affect most of the tissues in the body. In rheumatoid arthritis and many other types of inflammatory arthritis, the cartilage is characteristically destroyed evenly across all joint surfaces of both glenohumeral joints. The glenoid is eroded medially rather than posteriorly, as in degenerative joint disease. The arthritic process erodes not only cartilage but also subchondral bone, rendering it osteopenic and at risk for fracture
Rheumatoid and Other Types of Inflammatory Arthritis
Rheumatoid arthritis is a systemic disease with highly variable clinical manifestations. It can appear to be isolated to the glenohumeral joints or can affect most of the tissues in the body. In rheumatoid arthritis and many other types of inflammatory arthritis, the cartilage is characteristically destroyed evenly across all joint surfaces of both glenohumeral joints. The glenoid is eroded medially rather than posteriorly, as in degenerative joint disease. The arthritic process erodes not only cartilage but also subchondral bone, rendering it osteopenic and at risk for fracture
Rheumatoid arthritis can be associated with major bone loss and rotator cuff deficiency even in young individuals
When the onset of the disease occurs during youth, the joint volume may be small and the humerus curved with a thin medullary canal.
The restoration of comfort and function to the rheumatoid glenohumeral joint is often complicated by concurrent involvement of the rotator cuff as well as the acromioclavicular, sternoclavicular, elbow, wrist, and hand articulations and the joints of the opposite upper extremity. Arthritis in the lower extremities may demand the use of ambulatory aids or wheelchair transfers by the affected upper extremities. Even the skin of the individual with rheumatoid arthritis may be fragile and subject to compromise in wound healing. The fragility of a patient with rheumatoid arthritis is often compounded by long-term use of steroids and other antimetabolic medications. The condition itself involves the immune system, the patient is often receiving immunosuppressive medication, and the clinical manifestations of rheumatoid arthritis are similar to those of infectious arthritis; therefore, the physician must be aware of the possible coexistence of joint infection. Methotrexate may also increase the risk of nerve dysfunction after shoulder arthroplasty.
Because of the fragility of the skin and other soft tissues, osteopenia, and severe bone erosion common with this condition, a patient with substantial involvement of rheumatoid arthritis or similar types of arthritis must be treated with extreme gentleness and thoughtfulness. Shoulder arthroplasty for rheumatoid arthritis has a high rate of glenoid component loosening and rotator cuff failure. Patients with rheumatoid arthritis characteristically have substantially lower self-assessed vitality and overall physical function than do those with other causes of glenohumeral arthritis. The compromised general health and strength of patients with rheumatoid arthritis must be considered in planning their surgical and postoperative management. Special preoperative evaluation and intraoperative care are directed at the potentially tenuous stability of the cervical spine.
Cuff Tear Arthropathy
Cuff tear arthropathy is a compound degenerative condition of the shoulder that involves tendon, cartilage, and bone. In this condition chronic, massive rotator cuff defects are associated with loss of the humeral articular cartilage and superior displacement of the humeral head so that it articulates with the undersurface of the coracoacromial arch We say that the humeral head becomes “femoralized” by rounding off of the tuberosities while the coracoacromial arch and upper glenoid fossa become “acetabularized” when the humerus sculpts a concentric concavity from these structures.
In cuff tear arthropathy, the glenohumeral joint is deprived of several of its major stabilizing factors: the normal cuff muscle force vector compressing the humeral head into the glenoid; the superior lip of the glenoid concavity, which is typically worn away by chronic superior subluxation and the cuff tendon that is normally interposed between the humeral head and the coracoacromial arch. The superior displacement of humeral head slackens the deltoid so that its ability to flex or abduct the shoulder is weakened. With progression of the condition, the coracoacromial arch may become compromised, allowing anterior superior escape. Previous acromioplasty and section of the coracoacromial ligament further compromise glenohumeral stability and contribute to anterosuperior escape. The consequences of loss of integrity of the coracoacromial arch remind us of the need to preserve the integrity of the acromion and coracoacromial ligament in all shoulder procedures.
Cuff tear arthropathy provides several challenges for the surgeon. In the absence of an intact rotator cuff, total shoulder arthroplasty has been shown to have an early failure rate from glenoid loosening through what we have described as the “rocking horse phenomenon”. Standard hemiarthroplasty may provide only partial pain relief and partial improvement in function. Currently either a cuff tear arthropathy prosthesis or a reverse total shoulder is commonly used in the surgical management of cuff tear arthropathy. Several different systems for the classification of the pathoanatomy of cuff tear arthropathy have been proposed as guides to treatment. However more than radiographic classification, we have found the critical factors in determining treatment to be (1) the stability of the humeral head beneath the coracoacromial arch (i.e. the presence or absence of anterosuperior escape), (2) the amount of active elevation provided by the deltoid (i.e. the presence or absence of pseudoparalysis, which we define as the inability to actively raise the arm to 90 degrees in spite of good passive range of motion), (3) the strength of the residual internal and external rotator musculature, (4) the amount and quality of glenoid, humeral and acromial bone stock available for surgical reconstruction, (5) the patient’s fall risk (this is a particular concern in individuals with Parkinson’s disease or other problems of balance), (6) the patient’s dependency on the upper extremities for mobility, and (7) the patient’s activity expectations.
Avascular Necrosis
Nontraumatic or primary avascular necrosis of the humeral head may be idiopathic or may be associated with systemic steroids, trauma, dysbaric conditions, renal or other organ transplantation, or systemic illnesses with vasculitis. Other implicated conditions include alcoholism, sickle cell disease, hyperuricemia, Gaucher’s disease, pancreatitis, familial hyperlipidemia, and lymphoma. Avascular necrosis has also been reported as a result of section of the anterior humeral circumflex humeral artery in open instability surgery.
Avascular necrosis of the humeral head may be seen on plain films or MRI before collapse of the joint surface occurs. Often a fracture through the abnormal subchondral bone superocentrally is noted. Subsequently, collapse of the subchondral bone can occur, putting the glenoid articular surface at risk for secondary erosion. In end-stage avascular necrosis, the irregular humeral head destroys glenoid articular cartilage and thereby results in glenohumeral joint disease.
Because of the fragility of the skin and other soft tissues, osteopenia, and severe bone erosion common with this condition, a patient with substantial involvement of rheumatoid arthritis or similar types of arthritis must be treated with extreme gentleness and thoughtfulness. Shoulder arthroplasty for rheumatoid arthritis has a high rate of glenoid component loosening and rotator cuff failure. Patients with rheumatoid arthritis characteristically have substantially lower self-assessed vitality and overall physical function than do those with other causes of glenohumeral arthritis. The compromised general health and strength of patients with rheumatoid arthritis must be considered in planning their surgical and postoperative management. Special preoperative evaluation and intraoperative care are directed at the potentially tenuous stability of the cervical spine.
Cuff Tear Arthropathy
Cuff tear arthropathy is a compound degenerative condition of the shoulder that involves tendon, cartilage, and bone. In this condition chronic, massive rotator cuff defects are associated with loss of the humeral articular cartilage and superior displacement of the humeral head so that it articulates with the undersurface of the coracoacromial arch We say that the humeral head becomes “femoralized” by rounding off of the tuberosities while the coracoacromial arch and upper glenoid fossa become “acetabularized” when the humerus sculpts a concentric concavity from these structures.
In cuff tear arthropathy, the glenohumeral joint is deprived of several of its major stabilizing factors: the normal cuff muscle force vector compressing the humeral head into the glenoid; the superior lip of the glenoid concavity, which is typically worn away by chronic superior subluxation and the cuff tendon that is normally interposed between the humeral head and the coracoacromial arch. The superior displacement of humeral head slackens the deltoid so that its ability to flex or abduct the shoulder is weakened. With progression of the condition, the coracoacromial arch may become compromised, allowing anterior superior escape. Previous acromioplasty and section of the coracoacromial ligament further compromise glenohumeral stability and contribute to anterosuperior escape. The consequences of loss of integrity of the coracoacromial arch remind us of the need to preserve the integrity of the acromion and coracoacromial ligament in all shoulder procedures.
Cuff tear arthropathy provides several challenges for the surgeon. In the absence of an intact rotator cuff, total shoulder arthroplasty has been shown to have an early failure rate from glenoid loosening through what we have described as the “rocking horse phenomenon”. Standard hemiarthroplasty may provide only partial pain relief and partial improvement in function. Currently either a cuff tear arthropathy prosthesis or a reverse total shoulder is commonly used in the surgical management of cuff tear arthropathy. Several different systems for the classification of the pathoanatomy of cuff tear arthropathy have been proposed as guides to treatment. However more than radiographic classification, we have found the critical factors in determining treatment to be (1) the stability of the humeral head beneath the coracoacromial arch (i.e. the presence or absence of anterosuperior escape), (2) the amount of active elevation provided by the deltoid (i.e. the presence or absence of pseudoparalysis, which we define as the inability to actively raise the arm to 90 degrees in spite of good passive range of motion), (3) the strength of the residual internal and external rotator musculature, (4) the amount and quality of glenoid, humeral and acromial bone stock available for surgical reconstruction, (5) the patient’s fall risk (this is a particular concern in individuals with Parkinson’s disease or other problems of balance), (6) the patient’s dependency on the upper extremities for mobility, and (7) the patient’s activity expectations.
Avascular Necrosis
Nontraumatic or primary avascular necrosis of the humeral head may be idiopathic or may be associated with systemic steroids, trauma, dysbaric conditions, renal or other organ transplantation, or systemic illnesses with vasculitis. Other implicated conditions include alcoholism, sickle cell disease, hyperuricemia, Gaucher’s disease, pancreatitis, familial hyperlipidemia, and lymphoma. Avascular necrosis has also been reported as a result of section of the anterior humeral circumflex humeral artery in open instability surgery.
Avascular necrosis of the humeral head may be seen on plain films or MRI before collapse of the joint surface occurs. Often a fracture through the abnormal subchondral bone superocentrally is noted. Subsequently, collapse of the subchondral bone can occur, putting the glenoid articular surface at risk for secondary erosion. In end-stage avascular necrosis, the irregular humeral head destroys glenoid articular cartilage and thereby results in glenohumeral joint disease.
Early in course of the disease, core decompression may be of benefit. When the process involves only the humeral head, a humeral hemiarthroplasty is considered. When the glenoid is involved, a glenohumeral arthroplasty may be needed
Glenohumeral chondrolysis
This is a condition the etiology of which unfortunately was formerly referred to as being ‘speculative’, but is now clearly recognized as most commonly being caused by the intraarticular infusion of local anesthetics using a ‘pain pump’ – this condition is particularly a risk after arthroscopic procedures in which suture anchors were placed in the glenoid. Chondrolysis has also been associated with radiofrequency or laser procedures within the joint. The diagnosis is made from the history of pain pump use, the postoperative onset of pain and stiffness, and radiographs showing the loss of the joint space without osteophytes
Neurotropic (Charcot) arthropathy
This condition arises in association with syringomyelia, diabetes, or other causes of joint denervation. The joint and subchondral bone are destroyed because of loss of the trophic and protective effects of its nerve supply. Cervical spine trauma might have occurred in the past, or unrecognized syringomyelia might exist. Other causes include diabetes, leprosy, syphilis, and chronic alcoholism. It has been suggested that the injection of corticosteroids might accelerate the development of this condition. The Charcot joint is characterized by functional limitation and pain (despite the denervation). Significant bone destruction and osseous debris are usually present about the joint area.
To help remember the characteristic features, we use the pneumonic of the three “d”s: “denervation, destruction and debris”. This condition can resemble infectious arthritis. The longevity of an arthroplasty performed for Charcot arthropathy may be jeopardized by the lack of protective nerve supply.
Radiation arthropathy
This condition, especially for the treatment of breast cancer, can cause a number of shoulder problems: brachial plexopathy, osteonecrosis, secondary malignant bone tumors, and fibrous scaring. Glenohumeral cartilage and subchondral bone are occasionally affected by these changes and can require treatment by prosthetic arthroplasty. Lack of normal soft tissue suppleness, scars from prior surgery and lymphedema may complicate surgical management.
Septic arthritis
This condition of the shoulder may arise from bacteria in the patient’s dermis, from hematogenous spread from a remote infection or from injections in or surgery on the joint itself. Patients with reduced immunological defenses – from chronic systemic disease, or from immunosuppressive medications – are particularly at risk. Radiographs may show bone destruction and instability
Treatment must be directed at resolving the infection before arthroplasty can be considered in the management of the resulting arthritis.
Neoplastic joint destruction
This condition may present insidiously and is often characterized by nonmechanical pain, i.e. pain at rest. Alternatively, tumors may present acutely as a pathological fracture. The diagnosis will depend on knowledge of the patient’s general health, high-quality plain radiographs, and possibly additional imaging modes, such as tomography, CT, bone scanning, or MRI. Identification of the primary lesion in metastatic disease is desirable, but sometimes biopsy of the shoulder lesion is the most direct route when making a diagnosis.
Miscellaneous arthropathies
This group includes crystalline arthritis (calcium pyrophosphate deposition disease, hydroxyapatite deposition disease), dialysis arthropathy, hemophilic arthropathy, hemochromatosis, synovial chondrometaplasia, alkaptonuria, gouty arthropathy, acromegalic arthropathy, spondyloarthropathy, Milwaukee shoulder, amyloid arthropathy, pseudogout, primary hyperparathyroid arthropathy, psoriatic arthropathy, ulcerative colitis, Crohn’s disease, Reiter’s syndrome, pigmented villonodular synovitis, Lyme arthritis, and rapidly destructive articular disease
Videos on the surgical treatments for shoulder arthritis can be found on these links:
total ahoulder arthroplasty
ream and run arthroplasty
cuff tear arthropathy arthroplasty
reverse total shoulder arthroplasty
=====
How you can support research in shoulder surgery Click on this link.
To see our new series of youtube videos on important shoulder surgeries and how they are done, click here.
Use the "Search" box to the right to find other topics of interest to you.How you can support research in shoulder surgery Click on this link.
To see our new series of youtube videos on important shoulder surgeries and how they are done, click here.
You may be interested in some of our most visited web pages arthritis, total shoulder, ream and run, reverse total shoulder, CTA arthroplasty, and rotator cuff surgery as well as the 'ream and run essentials'