Deconflicting use of the term "subluxation".
Most orthopaedic surgeons use the word subluxation to refer to separation of the surfaces of a joint, as in patello-femoral subluxation
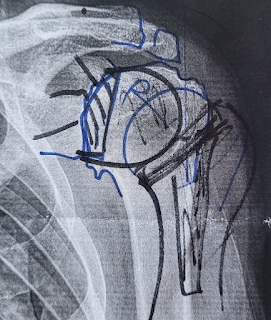
Consistent with Walch's classic article, the authors of Quantitative Measurement of Osseous Pathology in Advanced Glenohumeral Osteoarthritis defined subluxation in terms of "humeroglenoid alignment" or HGA, and found that the humeral head was relatively well centered in the retroverted B3 type compared with the type B2 glenoid.
However, as pointed out in Subluxation in the Arthritic Shoulder many authors have recently confused the use of the word "subluxation" by using it to refer to alignment of the humeral head with the scapular axis, rather than with respect to the plane of the glenoid face. The relationship of the humeral head to the plane of the scapula is mostly determined by glenoid retroversion and is not a measure of glenohumeral subluxation.
Interestingly, the authors of Progression of Glenoid Morphology in Glenohumeral Osteoarthritis found that arthritic shoulders that started out with the humeral head centered with respect to the plane of the glenoid face rarely progressed to becoming subluxated (i.e. decentered).
Does glenoid version need "correcting"
If humeral head decentering on the glenoid face is not driven by glenoid retroversion, is it necessary to "correct" glenoid retroversion when performing a shoulder arthroplasty?
The authors of Does glenoid version and its correction affect outcomes in anatomic shoulder arthroplasty? A systematic review found that "there is currently insufficient evidence that pre- or postoperative glenoid version influences postoperative outcomes independent of other morphologic factors such as joint line medialization. Given that noncorrective reaming demonstrated favorable postoperative outcomes, and that postoperative glenoid version was not significantly and consistently found to impact outcomes, there is inconclusive evidence that correcting glenoid retroversion is routinely required."
Anatomic total shoulder arthroplasty for posteriorly eccentric and concentric osteoarthritis: a comparison at a minimum 5-year follow-up found that the results of TSA with conservative glenoid reaming without attempt at version correction were favorable at a minimum 5- year, and mean 8-year, follow-up. There were no differences in clinical and radiographic outcomes between patients with eccentric and concentric wear patterns. Incomplete glenoid component seating was the greatest predictor of glenoid component radiolucency.
Does Postoperative Glenoid Retroversion Affect the 2-Year Clinical and Radiographic Outcomes for Total Shoulder Arthroplasty? noted that postoperative glenoid retroversion was not associated with inferior clinical results at 2 years after surgery.
Glenoid subchondral bone density distribution in male total shoulder arthroplasty subjects with eccentric and concentric wear pointed out that attempts to correct glenoid version may result in loss of the dense glenoid bone that contributes to good fixation of a glenoid component.
The authors Management of intraoperative posterior decentering in shoulder arthroplasty using anteriorly eccentric humeral head components showed that decentering of the humeral head with respect to the plane of the glenoid face could be corrected without changing glenoid version through the use of an anteriorly eccentric humeral head component
.
How do anatomic and reverse total shoulders compare in the treatment of glenohumeral arthritis with an intact cuff?
A comparative analysis of anatomic total shoulder arthroplasty versus reverse shoulder arthroplasty for posterior glenoid wear patterns noted that patients with shoulder osteoarthritis and posterior glenoid wear patterns with an intact rotator cuff who underwent TSA had similar outcomes as RSA. The TSA group had superior active external rotation and internal rotation at 2 years postoperative compared with RSA.
Treatment of B2 Type Glenoids with Anatomic versus Reverse Total Shoulder Arthroplasty: A Retrospective Review found that anatomic and reverse total shoulder arthroplasty can produce good results in patients with B2 glenoid morphology with low rates of revision with appropriate patient selection. Anatomic total shoulder arthroplasty may result in improved range of motion.
Survivorship of shoulder arthroplasty in young patients with osteoarthritis: an analysis of the Australian Orthopaedic Association National Joint Replacement Registry noted that instability/dislocation were the leading causes of revision for RTSA (41.7%) For TSA, the majority of revisions were for either instability/dislocation (20.6%) or loosening (18.6%).The high early dislocation rate associated with RTSA, as well as the lack of revision options available to address this, indicates that careful selection of patients and a greater appreciation of anatomic risk factors are needed in the future.
Total Shoulder Arthroplasty Versus Reverse Shoulder Arthroplasty in Primary Glenohumeral Osteoarthritis With Intact Rotator Cuffs: A Meta-Analyses in the setting of primary glenohumeral osteoarthritis with an intact cuff reverse total shoulder were found to be non-inferior to the TSA.
The Influence of Rotator Cuff Disease on the Results of Shoulder Arthroplasty for Primary Osteoarthritis demonstrated that minimally retracted or nonretracted rotator cuff tears limited to the supraspinatus tendon do not appreciably affect most shoulder-specific outcome parameters in total shoulder arthroplasty performed for the treatment of primary osteoarthritis. Conversely, fatty degeneration of the infraspinatus and, less importantly, subscapularis musculature adversely affects many of these parameters.
Reverse total shoulder challenges
Development, Evolution, and Outcomes of More Anatomical Reverse Shoulder Arthroplasty presents the evolution of RSA design, particularly the development of a lateralized center of rotation constructs, which aimed to address the disadvantages associated with the Grammont-style design and more closely reproduce the native anatomy in order to improve patient outcomes in an expanded context of pathologies.
Glenoid morphology in reverse shoulder arthroplasty: Classification and surgical implications showed that abnormal glenoid morphology has a significant effect on anatomical and surgical factors which can necessitate adjustments in surgical technique for reverse shoulder arthroplasty including the use or the alternative spine centerline.
Implant-Positioning and Patient Factors Associated with Acromial and Scapular Spine Fractures After Reverse Shoulder Arthroplasty noted that while the original indication for a reverse total shoulder was cuff tear arthropathy with pseudoparalysis, patients with this condition have inferior outcomes in comparison to those with intact rotator cuffs. Poor bone density and rotator cuff deficiency appear to be the strongest predictors of acromial and scapular spine fractures after RSA. To a lesser degree, increased humeral lateralization appear to be associated with lower fracture rates while glenoid-sided and global lateralization are associated with higher fracture rates. However, glenoid lateralization may improve shoulder stability, range of motion and function while reducing the risk of unwanted prosthesis-bone contact with associated limitations in range of motion and scapular notching.
An alternative approach to cuff tear arthropathy.
Cuff Tear Arthropathy: Pathogenesis, Classification, and Algorithm for Treatment showed that the use of an extended humeral head prosthesis for Types-IA, IB, and IIA cuff tear arthropathy revealed substantial improvement in pain relief, range of motion, and functional goals.
Managing rotator cuff tear arthropathy: a role for cuff tear arthropathy hemiarthroplasty as well as reverse total shoulder arthroplasty showed that for patients having cuff tear arthropathy with retained active elevation, an extended head humeral hemiarthroplasty yielded clinically important improvement in comfort and function while avoiding the complications of dislocation and acromial/spine fracture that can be associated with a reverse total shoulder.
New technologies
Assessing the Value to the Patient of New Technologies in Anatomic Total Shoulder Arthroplasty The analysis did not identify evidence that the results of TSA were statistically or clinically improved over the 2 decades of study or that any of the individual technologies were associated with significant improvement in patient outcomes.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link)
Shoulder rehabilitation exercises (see this link).