A number of recent articles have espoused the importance of "restoring premorbid bony shoulder anatomy" when performing total shoulder arthroplasty, including Prediction of premorbid three-dimensional anatomy of the glenoid based on statistical shape modeling, Premorbid glenoid anatomy reconstruction from contralateral shoulder 3-dimensional measurements: a computed tomography scan analysis of 260 shoulders, and Three-dimensional analysis of biplanar glenoid deformities: what are they and can they be virtually reconstructed with anatomic total shoulder arthroplasty implants?
When the preoperative bony anatomy is essentially normal (e.g. type A1 pathoanatomy) the amount of planned change in glenoid joint line is small (compare calculated premorbid anatomy (yellow) to the preoperative anatomy (superimposed CT image).

However, with more advanced forms of pathoanatomy (e.g. a B3 glenoid), restoring premorbid anatomy will push the humerus laterally from where it was preoperatively and tighten the shoulder.
Here are some examples of different plans designed to restore premorbid anatomy, each with the same effect: pushing the humeral head laterally.
The lateral pushing of the humerus to achieve premorbid anatomy may seem compelling from the boney perspective; however in glenohumeral arthritis the soft tissues (capsule, subscapularis, and rotator cuff) surrounding the glenohumeral joint are not in their premorbid state, but rather contracted and stiff - even after vigorous soft tissue releases. Thus restoring premorbid bony anatomy of the glenoid (and humeral head) may functionally overstuff the shoulder as originally described in the (freely downloadable) 1990 Practical Evaluation and Management of the Shoulder and as shown in the figure below

and as discussed in detail in Overstuffing is not a radiographic diagnosis. Overstuffing is not a condition diagnosed on x-ray, rather it is a condition in which there is too much stuff in the available space within the glenohumeral joint. Sort of like what Lewis Carroll described in his 1865 children's novel, Alice in Wonderland. After Alice drinks from the bottle labeled "DRINK ME" she expands to where she cannot move.
The function of the shoulder depends on its mobility and stability as discussed by many prominent authors in a 1993 AAOS publication I had the pleasure of editing with my friends Rich Hawkins and the late Freddie Fu.
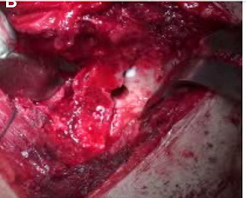
No amount of preoperative planning can assure that the postoperative shoulder has a balance of mobility and stability: the shoulder we have in the operating room after osteophyte resection and soft tissue releases is not the same shoulder the patient had in the preoperative area.
My approach is to conservatively ream the glenoid just enough to achieve 100% backside contact and excellent seating of a standard glenoid component; preserving glenoid bone stock without worrying about "correcting" glenoid version (see "accepting glenoid retroversion") and without worrying about peg penetration (NB: with modern peg configuration, cortical peg penetration may actually enhance fixation).
Once the glenoid component is fixed and well seated, the "best guess" humeral trial component is inserted based on both preoperative planning and on the amount of preoperative shoulder stiffness.
The shoulder is then checked to be sure that
(1) the mobilized subscapularis reaches the lesser tuberosity with the arm in 40 degrees of external rotation
(2) the range of motion includes 150 degrees of flexion and 60 degrees of internal rotation with the arm in 90 degrees of abduction
(3) the humeral head is translatable posteriorly by 50 percent of the width of the glenoid and returns to the centered position when the translating force is removed ("spring back aka springbok").
(4) when the arm is held in 90 degrees of flexion and shaken, the humeral head translates no more than 50 percent of the width of the glenoid ("shake and bake").
If the shoulder is too tight, the head thickness downsized. If the shoulder has excessive posterior translation or internal rotation or is posteriorly unstable when the arm is flexed to 90 degrees, an anteriorly eccentric humeral head component is considered as shown in this post.
These kinematic modifications of the preoperative plan do not attempt to recreate the premorbid anatomy, but rather are designed restore the lost premorbid function - motion and stability - while preserving the precious glenoid bone stock.
Getting the best functioning total shoulder for each of our patients is a big ask, but we need to keep working at it.
Mt Rainier
July 6, 2025
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link)
Shoulder rehabilitation exercises (see this link).































-topaz-denoise.jpg)