Stay curious
Anatomic total shoulder arthroplasty - aTSA (rather than reverse total shoulder - RSA) is for many surgeons the "go to" procedure for most patients with cuff-intact shoulder arthritis. While in the past there have been concerns about (1) glenoid component failure and (2) failure of the rotator cuff, modern glenoid implants and improved surgical techniques to assure excellent glenoid component seating along with proper preoperative evaluation of the rotator cuff have greatly reduced these risks. It is well documented that the range of motion is on average better for aTSA than RSA and that in contrast to RSA, aTSA essentially avoids the risks of two serious complications of RSA: dislocation and acromial/spine fractures. While some studies have shown lower revision rates for RSA than aTSA, these studies must be viewed from the perspective that in the uncommon occurrence of aTSA failure, a revision to an RSA is usually successful. However revision for an unstable RSA or an acromial/spine fracture may be avoided by the patient and surgeon because of concerns about complications and effectiveness.
An informative study on aTSA in the management of two common forms of osteoarthritis can be found in Anatomic total shoulder arthroplasty for posteriorly eccentric and concentric osteoarthritis: a comparison at minimum 5-year follow-up. This article presents outcomes for aTSA performed using an all-polyethylene glenoid component inserted after conservative glenoid reaming with no attempt at changing glenoid version. Two hundred and ten patients were included of which 98 (47%) had posteriorly decentered humeral heads and 108 (51%) had centered humeral heads. 77 shoulders had Walch type A glenoids; 122 had Walch type B glenoids. At a mean 8-year follow-up, the final SST, change in SST and percentage of maximal improvement were not correlated with pre- or postoperative humeral head centering on the glenoid, Walch classification or glenoid version. Two patients (1%) underwent open re-operations during the study period. In patients with Walch B1 and B2 glenoids (n=110), there were no differences in outcome measures between patients with postoperative glenoid component retroversion of more or less than 15o. While 15 of 51 patients (29%) with 5-year radiographs had glenoid radioluciences, these radiographic findings were not associated with inferior clinical outcomes. On multivariable analysis glenoid component radiolucencies were most strongly associated with incomplete component seating.
Risk of complications:
A Preoperative Risk Assessment Tool for Predicting Adverse Outcomes among Total Shoulder Arthroplasty Patients studied 208,634 TSAs performed on Medicare-insured patients. More than one in ten (11.2%) had at least one adverse outcome (hospital readmission, postoperative complication, emergency room visit, or mortality during the 90 days post discharge). Patients with an adverse outcome were older, more likely to be female, have a diagnosis of fracture, issues related to social determinants of health, greater healthcare utilization, and comorbidities such as anemia. Notably, this study did not identify surgical technical factors related to adverse outcomes.
Risk factors for rotator cuff tears and aseptic glenoid loosening after anatomic total shoulder arthroplasty reviewed 2699 primary aTSAs (1823F/ 1,922M/27 unspecified; mean age: 65.6 years). 5 different glenoid design types were used (1779 nonaugmented hybrid cage glenoid components, 650 posterior augment cage, 731 nonaugmented peg, 212 posterior augment peg, 369 keel, and 31 unspecified). The indications for the different glenoid types was not specified. 3.2% aTSA shoulders had a cuff tear. The multivariate analysis identified that aTSA patients with cuff failure were more likely to have previous shoulder surgery and small size glenoids. 3.3% of aTSA shoulders had aseptic glenoid loosening; 15.5% loose glenoids also had a rotator cuff tear. 30 of the 123 glenoid failures were cage-glenoid dissociations. The multivariate analysis identified that aTSA patients with aseptic glenoid loosening were more likely to be younger (≤62 years) at the time of surgery, have small size glenoids and have a nonhybrid glenoids.
Glenoid Components:
As the study above indicates, some glenoid implants use hybrid fixation - often with a metallic central post.
Ten-Year Implant Survivorship and Performance of Anatomic Total Shoulder Arthroplasty Patients with the Zimmer Biomet Comprehensive® Shoulder System - a Short Stemmed Humeral Implant and Hybrid Glenoid concluded that patients having hybrid glenoid components had comparable long-term clinical results in comparison to the current longitudinal literature regarding survivorship of other implant systems.
Some authors advocate metal-backed glenoid components; yet a number of studies, point to a higher revision rate for these implants.
High revision rate of metal-backed glenoid component and impact on the overall revision rate of stemless total shoulder arthroplasty: a cohort study from the Danish Shoulder Arthroplasty Registry found that for the Eclipse stemless TSA system, the adjusted hazard ratio for revision of a metal-backed glenoid component was 8.75 in comparison to stemless Eclipse with an all-polyethylene glenoid component.
There is interest in the effect of the type of polyethylene used: cross linked, XLPE or non cross linked, non-XLPE. While many favor XLPE the article below emphasized the importance of controlling for other variables that can affect component longevity
Modelling XLPE vs non-XLPE glenoid revision rates for anatomic shoulder arthroplasty in osteoarthritis including differing polyethylene glenoid fixation designs. found that when restricted to procedures performed since 2017 there was no significant association between polyethylene type and revision rates after adjustment for patient age, sex, humeral head size, humeral fixation, stemmed or stemless and glenoid component type (metal backed, cemented polythylene, or all polyethylene with a modified central peg).
Keeled components are going out of favor, yet this 10 year followup of young patients is of interest.
Anatomical Total Shoulder Arthroplasty with Keeled glenoids in Patients under 60 years at 10 years minimum: which risk factors of failure are still valid at long term follow-up? 87 shoulders in 82 patients 36 to 60 yo were included at a mean follow-up of 14 years. Revision-free survivorship was 81% at 10 years and 65% at 15 years. Among the 28 revised shoulders, 19 were for glenoid loosening. Heavy labor was a risk factor for glenoid component loosening. While Walch type did not influence revision rate, flat backed components and glenoids prepared with curettage (rather than reaming) were risk factors for glenoid. This reinforces the concept that glenoid component seating is an essential element for preventing loosening.
Some authors advocate for posteriorly augmented glenoid components in shoulders with posterior bone loss.
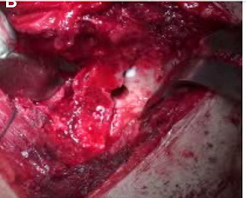
Total shoulder arthroplasty for glenohumeral arthritis associated with posterior glenoid bone loss: midterm results of an all-polyethylene, posteriorly augmented, stepped glenoid component. presents the use of a stepped glenoid component which requires the removal of some posterior glenoid bone as shown here.
Thirty-five shoulders with minimum 5-year follow-up underwent aTSA using a posteriorly augmented glenoid component for the treatment of glenohumeral osteoarthritis with posterior glenoid bone loss. Postoperative Grashey and axillary radiographs were reviewed to record the degree of radiolucency surrounding glenoid pegs on a scale of 0 (no radiolucency) to 5 (gross loosening), as described by Lazarus et al. The degree of central peg osseous integration was classified via x-ray on a scale of 1 to 3, as described by Wirth et al, with 3 representing complete integration and 1 indicating surrounding osteolysis. Survivorship free from revision was 92% at 8.8 years postoperatively. Two patients experienced prosthetic instability requiring revision, leaving 33 shoulders with an average follow-up of 6.6 years. There was a progressive increase in Lazarus score and a decrease in Wirth score between 2- and 5-year follow-up. A significant correlation was identified between VAS pain scores and both Lazarus and Wirth scores, i.e. the severity of radiographic loosening correlated with subjective pain levels. The authors concluded that these outcomes were comparable ("noninferior") to those for patients undergoing TSA with a nonaugmented glenoid component for the treatment of posterior glenoid bone loss as reported in the literature.
There is increasing interest in stemless humeral components
Influence of humeral position of the Affinis short® stemless shoulder arthroplasty system on long-term survival and clinical outcome reviewed 80 patients treated with a stemless shoulder arthroplasty for OA of the shoulder at a mean follow-up of 92 months. Range of motion and outcome scores were improved. The center of rotation restoration was anatomical in 75 % of all implants and in non-anatomical in 25 %. The humeral component position did not affect the functional outcome whereas the ten-year cumulative survival rate for the anatomic group was higher in comparison with the non-anatomical group (96.7 % vs. 75 %).
Analysis of Factors Influencing Optimal humeral sided Reconstruction in Anatomic Total Shoulder Arthroplasty reviewed 298 patients who underwent anatomic total shoulder arthroplasty (aTSA) utilizing three stem types: 145 long stem, 102 short stem, and 51 stemless implants. The stemless implant was more replicable in recreating the anatomic shape with a mean COR shift of 3.0 mm and neck shaft angle of 137. Stemless arthroplasty was also quicker to master compared to standard or short stemmed implants but did have a greater initial operative time.
The Effect of Lateralization on Clinical Outcomes after Anatomic Total Shoulder Arthroplasty found that the shift in center of rotation from the position determined by the "perfect circle" was the radiographic measure most closely associated with the ASES score, the WOOS score, and forward flexion.
The Impact of Three-Dimensional Humeral Planning and Standard Transfer Instrumentation on Reconstruction of Native Humeral Anatomy for Anatomic Total Shoulder Arthroplasty To explore the utility of planning and transfer instrumentation in inserting a stemless component, three surgeons used 3D-printed humeri based on CTs of existing patients. Humeral neck cuts were performed on all specimens (phase 1) without any preoperative humeral planning; (phase 2) with 3D planning, and (phase 3) with a neck-shaft angle (NSA) guide and digital calipers used to measure humeral osteotomy thickness to aid in the desired humeral cut. For both 3D change in center of rotation (COR) and medial to lateral change in COR, use of preoperative planning alone and with standard transfer instrumentation resulted in a more anatomic restoration of ideal COR. The deviations from planned cut thickness decreased with each phase: phase 1: 2.6 ± 1.9 mm, phase 2: 2.0 ± 1.3 mm, phase 3: 1.4 ± 0.9 mm (P = .041 for phase 3 vs. phase 1). For neck shaft angle, in phase 1, 7 of 15 (47%) cases were in varus; in phase 2, 5 of 15 (33%) were in varus; and in phase 3, 1 of 15 (7%) cases was in varus.
Rotator Cuff
Preoperative Rotator Cuff Fatty Infiltration and Muscle Atrophy Do Not Negatively Influence Outcomes Following Anatomic Total Shoulder Arthroplasty sought to determine the effects of rotator cuff fatty infiltration (FI) and muscle atrophy (MA) on clinical outcomes following TSA. There were 163 shoulders from 154 patients with a mean age of 62.5 and a mean follow-up of 2.9 years that met inclusion criteria. Rotator cuff muscle area was not correlated with any preoperative or postoperative range of motion or patient reported outcome measures. No significant differences in preoperative ROM or PROMs were found between patients with minimal-to-mild and moderate-to-severe FI (P > .05).
Methylprednisolone taper is an effective addition to multimodal pain regimens after total shoulder arthroplasty: results of a randomized controlled trial: 2022 Neer Award winner Patients were randomly assigned to receive intraoperative dexamethasone only (control group n=32) or intraoperative dexamethasone followed by a 6-day oral methylprednisolone (Medrol) taper course (treatment group n=35). The treatment group demonstrated a reduction in mean VAS pain scores over the first 7 postoperative days (POD). Between POD 1 and POD 7, patients in the control group consumed an average of 17.6 oxycodone tablets while those in the treatment group consumed an average of 5.5 tablets. This equated to oral morphine equivalents of 132.1 and 41.1 for the control and treatment groups, respectively. There were fewer opioid-related side effects during the first postoperative week in the treatment group. The treatment group reported improved VAS pain scores at 2-week, 6-week, and 12-week postoperatively. At follow-up there was 1 infection in the control group and 1 postoperative cubital tunnel syndrome in the treatment group.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link)
Shoulder rehabilitation exercises (see this link).
.












 or
or





