These authors reviewed patients infected with P. acnes after total hip (12 cases), knee (18 cases) and shoulder (35 cases) arthroplasty. Patients were included if they met the Musculoskeletal Infection Society criteria and were excluded if they had a polymicrobial culture. 74% of these patients were men.
Median ESR was significantly higher in the knee (38.0mm/h, IQR 18.0–58.0) and hip (33.5 mm/h, IQR 15.3–60.0) groups compared to the shoulder group (11.0 mm/h, IQR 4.5–30.5).
C-reactive protein levels were higher in the knee (2.0 mg/dl, IQR 1.3–8.9) and hip(2.4 mg/dl, IQR 0.8–4.9) groups compared to the shoulder group (0.7 mg/dl, IQR 0.6–1.5).
Median synovial fluid WBC was significantly higher in the knee group than shoulder group (19,950 cells/mm3, IQR 482–60,063 vs 750 cells/mm3, IQR 0–2825, respectively).
Peripheral blood WBC levels were similar between groups, as was mean time of P. acnes growth in culture.
Clindamycin resistance was present in all groups.
The authors concluded that "the manner in which a patient with P. acnes PJI presents is joint specific. Inflammatory markers were significantly higher in the knee and hip groups compared to the hip and shoulder groups, and long hold anaerobic cultures up to 14 days are necessary to accurately identify this organism."
Comment: This study indicates that knee and hip surgeons must join shoulder surgeons in being aware of the presence of Propionibacterium in the wounds of patients coming for revision arthroplasty. This study does not provide data on the rate of Propionibacterium identification in their revision surgery. It also does not indicate whether it is the routine of their surgeons to routinely send specimens for Propionibacterium-specific cultures. Unless cultures are sent and properly cultured, the presence of this organism will be missed.
This point is driven home by an article from 1999:
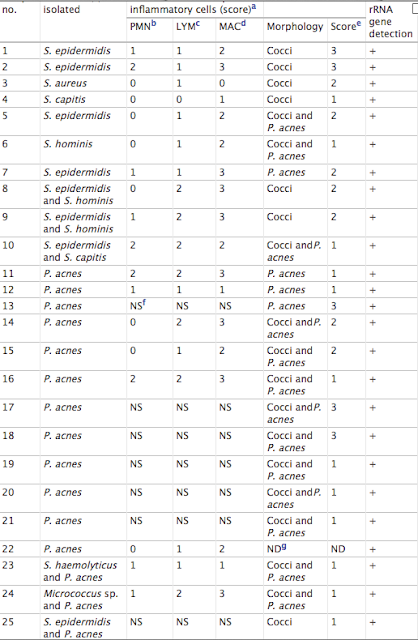
These authors compared the detection rates of bacterial infection of hip prostheses by culture and nonculture methods were compared for 120 patients with total hip revision surgery.
By use of strict anaerobic bacteriological practice during the processing of samples and without enrichment, the incidence of infection by culture of material dislodged from retrieved prostheses after ultrasonication (sonicate) was 22%.
Bacteria were observed by immunofluorescence microscopy in 63% of sonicate samples with a monoclonal antibody specific for Propionibacterium acnes and polyclonal antiserum specific for Staphylococcus spp. The bacteria were present either as single cells or in aggregates of up to 300 bacterial cells. These aggregates were not observed without sonication to dislodge the biofilm. Bacteria were observed in all of the culture-positive samples, and in some cases in which only one type of bacterium was identified by culture, both coccoid and coryneform bacteria were observed by immunofluorescence microscopy. Bacteria from skin-flake contamination were readily distinguishable from infecting bacteria by immunofluorescence microscopy. Examination of skin scrapings did not reveal large aggregates of bacteria but did reveal skin cells. These were not observed in the sonicates.
Bacterial DNA was detected in 72% of sonicate samples by PCR amplification of a region of the bacterial 16S rRNA gene with universal primers. All of the culture-positive samples were also positive for bacterial DNA. Evidence of high-level infiltration either of neutrophils or of lymphocytes or macrophages into associated tissue was observed in 73% of patients.
Note the prevalence Propionibacterium.
Their results indicate that the incidence of prosthetic joint infection is grossly underestimated by current culture detection methods.
====
Consultation for those who live a distance away from Seattle.
Click here to see the new Shoulder Arthritis Book.
Click here to see the new Rotator Cuff Book
Click here to see the new Shoulder Arthritis Book.
Click here to see the new Rotator Cuff Book
Information about shoulder exercises can be found at this link.
Use the "Search" box to the right to find other topics of interest to you.
You may be interested in some of our most visited web pages including:shoulder arthritis, total shoulder, ream and run, reverse total shoulder, CTA arthroplasty, and rotator cuff surgery as well as the 'ream and run essentials'
Use the "Search" box to the right to find other topics of interest to you.
You may be interested in some of our most visited web pages including:shoulder arthritis, total shoulder, ream and run, reverse total shoulder, CTA arthroplasty, and rotator cuff surgery as well as the 'ream and run essentials'