These authors used a 2-arm randomized, single blinded clinical trial to investigate the effectiveness of treating the subcutaneous tissue with povisdone-iodine (Betadine) in reducing the Cutibacterium culture rate in primary open shoulder surgery performed through a deltopectoral approach. 108 patients were enrolled in two groups (70 treatment vs 38 control).
The procedures included 32 open reductions and internal fixations, 67 total shoulder prostheses, and 9 shoulder stabilizations using an open Latarjet procedure.
A skin swab was taken for culture prior to standard surgical skin preparation.
After exposure of the deltoid fascia, the treatment group received preparation of the subcutaneous layer with povidone-iodine solution.
Once the proximal humerus was completely exposed, 5 swabs from different sites were taken for culture.
The subcutaneous Betadine treatment significantly reduced the positive culture rate of the operating field for all bacteria combined (p = 0.036) and specifically for Cutibacterium (p = 0.013).
The reduction of positive swabs for Cutibacterium was significant for the surgeon's gloves (p = 0.041) as well as for the retractors (p = 0.007).
37% of the control group and 19% of the treatment group showed at least 1 positive culture (any bacteria) for the deep cultures (RR=0.50, p = 0.036).
26% of the control group and 9% in the intervention group were deep culture positive for Cutibacterium (RR=0.33, p = 0.013)
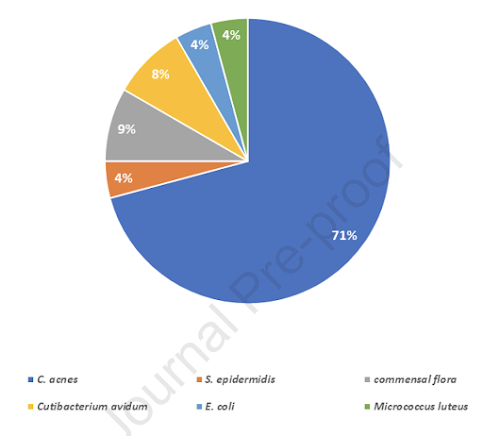
The percentages of the different bacteria in the cultures in the control group
These authors identified 5,534 primary THA and 6,204 primary TKA procedures. Cases were grouped on the basis of whether or not the wound was irrigated with 1 L of 0.25% Betadine prior to closure. Betadine irrigation was used in 1,322 (24%) of the THA cases and in 2,410 (39%) of the TKA cases.
Povidone-Iodine Wound Lavage to Prevent Infection After Revision Total Hip and Knee Arthroplasty An Analysis of 2,884 Cases
These authors assessed the effectiveness of Betadine irrigation in reducing infection following revision total hips (THA) and and total knees (TKA). Betadine lavage was employed in 27% of the revision THA cases and 34% of the revision TKA cases
They noted a trend toward higher rates for reoperation for infection among patients who received PI irrigation.
===
How you can support research in shoulder surgery Click on this link.
We have a new set of shoulder youtubes about the shoulder, check them out at this link.
Be sure to visit "Ream and Run - the state of the art" regarding this radically conservative approach to shoulder arthritis at this link and this link
Use the "Search" box to the right to find other topics of interest to you.