These authors report their outcomes for 54 consecutive patients with irreparable rotator cuff tears or pseudoparalysis (PPS) who underwent superior capsular reconstruction (SCR) using autologous tensor fascia lata with an average graft thickness of 8.3 mm.
The inclusion criterion for SCR was an irreparable rotator cuff tear or PPS with failed conservative treatment, supervised by physiotherapists, for >6 months. In all patients, the Hamada classification was grade 2 in 11 patients and grade 3 in 43 patients.
Included shoulders had a Goutallier grade 3 or higher fatty infiltration of the tendon with the tendon retracted to the glenoid level as evaluated on magnetic resonance imaging and torn tendons that could not reach the original footprint after the release of soft tissues at the time of surgery.
Pseudoparalysis (PPS) was defined as
(1) moderate PPS (n=16), no shoulder stiffness, active shoulder elevation (both flexion and abduction) ≤ 90 degrees , and the ability of the patient to maintain ≥ 90 degrees of elevation once the shoulder was passively elevated;
(2) severe PPS (n=16), comprising no shoulder stiffness, active shoulder elevation ≤ 90 degrees, and the inability of the patient to maintain ≥ 90 degrees of elevation once the shoulder was elevated passively; and
(3) non-PPS (n=22), comprising no shoulder stiffness and active shoulder elevation > 90 degrees.
Lidocaine was routinely injected into the subacromial space preoperatively; patients whose ROM improved were considered to have a painful loss of elevation and were not considered as patients with PPS.
Patients who could not elevate their shoulders even in the supine position were considered to have deltoid insufficiency and were excluded from this study.
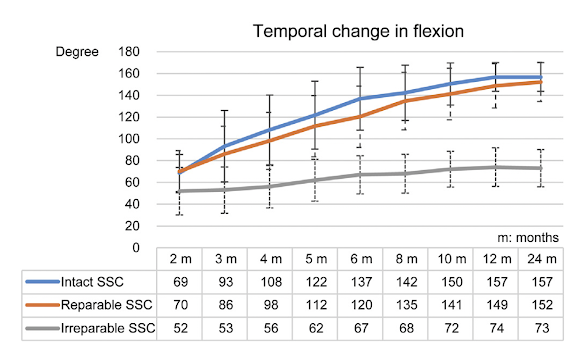
The 32 PPS patients were divided into 3 groups: intact subscapularis (SSC) (11 patients), repairable SSC (16 patients), and irreparable SSC (5 patients).
They found no significant differences in postoperative ASES scores and shoulder range of motion between the Hamada grade 2 and grade 3 groups or between the non-PPS, moderate PPS, and severe PPS groups. PPS patients required a longer duration to achieve shoulder elevation > 130 degrees; nevertheless, the authors found no significant differences in final outcomes between the non-PPS and PPS groups.
However, significant differences in postoperative ASES scores were observed between the intact SSC (final ASES = 91) and irreparable SSC groups (final ASES = 56) and between the repairable SSC (final ASES = 92) and irreparable SSC groups (final ASES = 56). There were significant differences in postoperative shoulder elevation (see graph below). The repairable SSC tear group tended to take longer to achieve improvement in shoulder elevation than the intact SSC group, although the final outcomes between the 2 groups did not show a significant difference.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
How you can support research in shoulder surgery Click on this link.
Here are some videos that are of shoulder interest