In performing anatomic total shoulder arthroplasty, some surgeons accept glenoid retroversion, inserting a standard glenoid component combined with techniques to maintain humeral head centering on the glenoid face while others prefer to change glenoid version (see Glenoid version: acceptors and correctors).
The clinical benefit of changing glenoid version for patients with shoulder arthritis is currently being investigated.
Glenoid components with thicker polyethylene posteriorly (see A, B, C and D below) have been used as a means of changing the version of the glenoid articular surface in anatomic total shoulder arthroplasty.
Glenoid components with thicker polyethylene posteriorly (see A, B, C and D below) have been used as a means of changing the version of the glenoid articular surface in anatomic total shoulder arthroplasty.
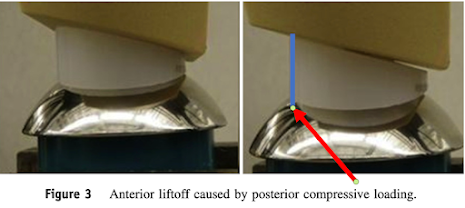
2013 The authors of Liftoff resistance of augmented glenoid components during cyclic fatigue loading in the posterior-superior direction used an in vitro model to measure the resistance to anterior glenoid liftoff when the posterior glenoid was eccentrically loaded by translating the humeral head 4 mm in the posterior-superior direction.
Each of the four augmented designs tested were less stable (i.e. showed greater micro motion with loading) than the standard, non-augmented glenoid component.
(1) the increased liftoff moment arm (blue line segment) resulting from the greater posterior thickness of the polyethylene as emphasized in 2019 Anatomic Augmented Glenoid Implants for the Management of the B2 Glenoid mentioning "concern for stresses generated in augmented implants", "glenoid augments tested in this study are at higher risk for loss of fixation and glenoid loosening because they were less resistant to liftoff", and "the stepped model showed higher levels of shear stress at both radial mismatch settings at the backside of the implant and in the cement mantle. Thus, while both designs performed similarly, the stepped design had high levels of stress, which indicates a higher risk for loosening, and higher amounts of micromotion in high-risk conditions."
and (2) from difficulty in fitting the bone to a complex component backside (below) in contrast to fitting a convex backed component to a spherically reamed bone surface.
The stabilizing effect of excellent bone carpentry and component seating is well recognized (see Edge displacement and deformation of glenoid components in response to eccentric loading. The effect of preparation of the glenoid bone and The radiographic evaluation of keeled and pegged glenoid component insertion.
The patient outcomes for the different approaches to the retroverted glenoid need to be compared by well-controlled clinical studies (see 2019 Augmented glenoid implants in anatomic total shoulder arthroplasty: review of available implants and current literature)
2015 Preliminary Results of a Posterior Augmented Glenoid Compared to an all Polyethylene Standard Glenoid in Anatomic Total Shoulder Arthroplasty reported on 24 patients with osteoarthritis and posterior glenoid wear who were treated with aTSA using a PAG with a minimum of two-year follow-up matched to patients treated with an all poly non-augmented pegged glenoid (NAG) for osteoarthritis. Sixty per-cent of PAG shoulders had a radiolucent line with an average radiographic line score of 1.10, and 33.3% of NAG had a radiolucent line with an average radiographic line score of 0.438. One glenoid in the PAG group was radiographically but not clinically loose. In the PAG group, 17/20 humeral heads were centered, and three were anteriorly subluxated; none were posteriorly subluxated. There were no differences in any of the measured postoperative clinical outcomes or any difference in improvement between the two groups.
2021 Stepped Augmented Glenoid Component in Anatomic Total Shoulder Arthroplasty for B2 and B3 Glenoid Pathology reported the use of a stepped augmented glenoid component to correct glenoid version for Walch B2 and B3 glenoids, comparing the radiographic and clinical outcomes at minimum 2-year follow-up with those achieved with a non-augmented component of the same design in Walch A1 glenoids.
Central peg osteolysis was graded as demonstrated below.
Range of motion and patient reported outcomes improved. Version was corrected. No patient had aseptic loosening. Seventy-nine of 86 patients had a Lazarus score of 0 (no radiolucency seen about peg or keel) at final follow-up.
2022 Early outcomes of augmented glenoid components in anatomic total shoulder arthroplasty: a systematic review found 9 studies including 312 shoulders underwent anatomic total shoulder arthroplasty using augmented glenoid implants. At an average of 37.1 months the average clinical outcome scores were improved. Glenoid retroversion was reduced from 21 to 9.5 degrees. Radiolucencies were reported in 35% of shoulders. The 16 degree full-wedge augment led to higher and more severe radiographic lucency, while high peg perforation rates (44%) were observed among 5-mm augment stepped implants. The overall rate of complication was 2.6%. Rate of revision surgery was 1.9%.
followed by full- wedge,
with the lowest amount of bone removal in half-wedge components.
The authors of 2023 Factors associated with functional improvement after posteriorly augmented total shoulder arthroplasty observed that posteriorly augmented glenoid components in anatomic total shoulder arthroplasty (TSA) address posterior glenoid bone loss with inconsistent results. They presented a retrospective review of 50 patients having TSA with a step-type augmented glenoid component at a minimum of 2 years after surgery. 41 had B2 glenoids while 9 had B3 glenoids.
One patient had center-peg osteolysis; 1 patient had glenoid component loosening. Postoperative glenoid component retroversion and residual posterior subluxation relative to the scapular body or glenoid face did not correlate with range of motion or shoulder function. However, humeral head decentering on the glenoid face was moderately associated with lower SANE scores.
2023 Clinical outcome of wedged glenoid reconstruction in anatomic total shoulder arthroplasty for osteoarthritic retroverted glenoid: a minimum 2-year follow-up reviewed 17 patients with a mean preoperative neoglenoid retroversion of 16.7°. The mean improvement was compared to a matched control group demonstrating a comparable magnitude of improvement.
Comment: Glenoid retroversion is common among patients having anatomic total shoulder arthroplasty, yet its importance in determining the outcome of joint replacement is not clear (see Prognostic Value of the Walch Classification for Patients Before and After Shoulder Arthroplasty Performed for Osteoarthritis with An Intact Rotator Cuff). Preoperative CT scans are now commonly used to measure retroversion and to plan its correction, yet the impact of 3D planning on clinical outcomes has not been rigorously determined (see Use of Preoperative CT Scans and Patient-Specific Instrumentation May Not Improve Short-Term Adverse Events After Shoulder Arthroplasty). The articles in the post demonstrate widely varying thresholds for the use of augmented components and little data on the clinical importance of version correction.
As shoulder surgeons we need to keep a keen eye on the strength of clinical evidence supporting the concept that correcting glenoid version and the frequent use of augmented glenoid components is of benefit to our patients. Consider for example the articles below.
2023 Does Glenoid Version and its Correction Impact Outcomes in Anatomic Shoulder Arthroplasty - a Systematic Review recognizes that while there are theoretical advantages to correction of glenoid retroversion in atomic total shoulder arthroplasty, limited information exists on the clinical benefit of correcting glenoid retroversion. The authors reviewed 16 studies evaluating the impact of glenoid retroversion on clinical and radiological outcomes of TSA; nine studies utilized corrective reaming techniques, four studies utilized posteriorly augmented glenoids, and two studies utilized non-corrective reaming techniques. Mean preoperative retroversion ranged from 12.7° to 24°. Eleven studies analyzed the effect of glenoid retroversion on clinical outcomes. The majority of the studies (8/11) did not report any significant association of pre- or postoperative glenoid retroversion on any clinical outcome. Of the three studies that reported significant effects, one study reported a negative association between preoperative glenoid retroversion and PROs, one study reported inferior postoperative abduction in patients with postoperative glenoid retroversion greater than 15 degrees, and one study found an increased clinical failure rate in patients with higher postoperative retroversion. Ten studies reported radiographic results (medial calcar resorption, central peg lucency (CPL) grade, Lazarus lucency grade) at follow-up. Only one study reported a significant effect of pre- and postoperative retroversion greater than 15 degrees on CPL grade. The authors concluded that there is currently insufficient evidence that pre- or postoperative glenoid version influences postoperative outcomes independent of other morphologic factors such as joint line medialization. Given that non-corrective reaming demonstrated favorable postoperative outcomes, and postoperative glenoid version was not significantly and consistently found to impact outcomes, there is inconclusive evidence that correcting glenoid retroversion is routinely required.
Furthermore, Early Radiographic and Clinical Outcomes of Primary Short Stem Anatomic Total Shoulder Arthroplasty with a Peripherally Enhanced Fixation Glenoid: A Multicenter Study "observed glenoid osteolysis in only 5.7% of cases with radiographic follow-up at median 28 months despite wide variation in preoperative glenoid morphology (52% B2 and B3 and only 25% A1)" without using any augmented glenoid components.
All of the above should prompt the search for better clinical evidence to support the currently common use of augmented glenoid components to correct glenoid version in anatomic total shoulder arthroplasty.
You can support cutting edge shoulder research and education that are leading to better care for patients with shoulder problems, click on this link.
Follow on twitter: https://twitter.com/RickMatsen or https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).