As emphasized in a recent post, acromial and scapular spine fractures continue to be a major cause of poor results after reverse total shoulder arthroplasty.
A couple of examples to kick things off.
Case 1: A 78 year old man had recognized risk factors for these fractures: osteoporosis and the diagnosis of cuff tear arthropathy. He has been treated for his osteoporosis with Alendronate.
His preoperative and post reverse total shoulder radiographs are shown below.
.
A month after surgery, while his arm was still in a sling immobilizer, he developed pain in his lateral shoulder. Examination revealed a localized spot of exquisite tenderness on the lateral acromion. On an axillary view a non-displaced crack is seen in his acromion at the site of his tenderness.
Case 2: An 82 year old woman had symptomatic cuff tear arthropathy and this AP radiograph
A reverse total shoulder was performed as shown below
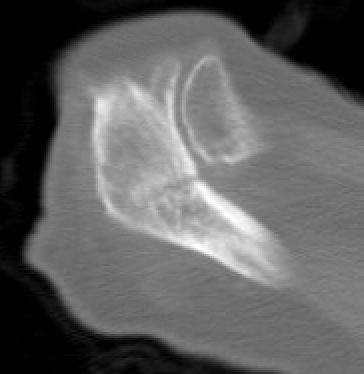
Two months after an uneventful recovery, she developed pain on use of the arm and point tenderness over the acromion posteriorly. While plain x-rays were unremarkable, a CT scan documented her stress fracture at the point of her tenderness
While these patients' age, sex, diagnoses of cuff tear arthropathy and osteoporosis were not modifiable, the question is whether there are modifiable risk factors, such as the geometry of the prosthetic RSA reconstruction.
A review of much of the current literature on this topic can be found in this post.
A recent publication, Shoulder Geometry After Reverse Total Shoulder Arthroplasty with a Medialized Glenoid and a Lateralized Humerus Predicts Subacromial Notching and Acromial or Scapular Spine Fractures, attempted to assess (1) whether the difference between the acromion to glenosphere center of rotation distance (DA) and the greater tuberosity to glenosphere center distance (DGT) influences the incidence of subacromial notching (SaN) in shoulders following reverse total shoulder arthroplasty (rTSA) and (2) whether this relationship is associated with the incidence of acromion or scapular spine fractures.
They conducted a retrospective cohort study of 526 patients who underwent RSA with a medialized glenoid and a lateralized humerus.
After propensity score matching, 360 shoulders were analyzed (240 in the DA ≥ DGT group and 120 in the DA < DGT group). Both groups showed similar improvements in clinical outcomes postoperatively.
The DA ≥ DGT group exhibited a significantly lower incidence of SaN (0%) compared to the DA < DGT group (10.8%, P < 0.001). Additionally, the DA ≥ DGT group had a lower rate of acromion or scapular spine fractures (0.4%) compared to the DA < DGT group (5.0%, P = 0.006) [although a larger sample size will be necessary to achieve statistical power].
If we go back to Case 1, the 78 year old man with the acromial fracture, his distance to acromion (green arrow) was ≥ distance to greater tuberosity (yellow arrow).

If we revisit Case 2, the 82 year old lady, her distance to acromion (green arrow) was ≥ the distance to greater tuberosity (yellow arrow).
These cases remind us that age, diagnosis of cuff tear arthropathy and osteoporosis are more strongly associated with the occurrence of acromion/spine fractures than component design or position. That said, patient demographics (female sex, age, rheumatoid arthritis) and shoulder diagnosis (cuff tear arthropathy, massive irreparable cuff tears with pseudoparalysis) are not modifiable, so we need to continue to research modifiable factors that may reduce the rate of these factors especially in high risk patients.
Possible candidates to be studied are (1) assuring that osteoporosis is under optimal management, (2) minimizing global lateralization of the humerus in RSA, (3) defining the optimal degree of glenosphere tilt and inferior placement, (4) burring down the lateral aspect of the greater tuberosity to make sure that there is no tuberosity/acromial contact when the arm is abducted and rotated, (5) slowing the return to activity after surgery, (6) prophylactic calcitonin, (7) considering a cuff tear arthropathy prosthesis rather than a RSA in high risk patients.
Jon Levy kindly responded to this post stating that his big three for minimizing the acromial / spine fracture risk are
(1) optimizing glenoid component fixation
(2) avoiding early arc abduction impingement (he currently uses 70 degrees as his goal post).
(3) avoiding lateralizing the final humerus position more than the preop position.We need to continue explore better methods for preventing these fractures: they are disabling for the patients that sustain them; they are too common.
Common Yellowthroat
Montlake Fill, April 2020
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link)
Shoulder rehabilitation exercises (see this link).