We strive to maintain the long head of the biceps tendon in performing shoulder arthroplasty unless it is frayed or unstable. While contrary to the opinion of some, we do not find that the biceps becomes a 'pain generator' after arthroplasty: specifically in our experience it is very rare for our patients with a "biceps-on" arthroplasty to have postoperative issues with their biceps tendon.
However at the time of arthroplasty, if the biceps is unstable or frayed, a tenodesis can easily be performed using what we call the 'in and out' technique.In this technique, we transect the biceps at its insertion to the supraglenoid tubercle, make a hole in the strong bone of the biceps groove about 5 cm below the humeral neck cut. The proximal end of the long head tendon is threaded through this hole and then brought out the neck cut. When the humeral component is driven into position, it robustly fixes the long head tendon so that no modification of the post operative rehabilitation is necessary.
Here's a photo from the OR. The patient had inflammatory arthritis with biceps tendon involvement. The lower blue arrow points to the hole in the bicipital groove with the tendon entering it. The upper blue arrow points to the tendon (with a single traction suture in it) exiting the medullary space where it will be fixed when the prosthesis is seated. The other six sutures have been placed for repair of the subscapularis.
And a diagram from Steve Lippitt
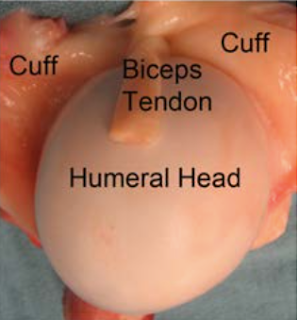
Here's another example from this week. At surgery the biceps tendon was flattened, frayed and unstable. After release from the supraglenoid tubercle, the biceps tendon was passed through a hole created in the cortical bone of the bicipital groove and then led out through the humeral neck cut. As the humeral prosthesis is inserted, the biceps tendon is tensioned by traction (see suture in the tendon at lower right). Seating the humeral implant secures the tendon. This technique adds minimal time to the case, avoids the challenge of placing a tenodesis screw, and avoids the potential tenuousness of suturing the tendon to soft tissue.
How you can support research in shoulder surgery Click on this link.
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The total shoulder arthroplasty (see this link).
The ream and run technique is shown in this link.
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
Shoulder rehabilitation exercises (see this link).
Follow on twitter: Frederick Matsen (@shoulderarth)