The long head tendon of the biceps (LHTB) is a component of normal shoulder structure and function. There are billions of people walking the earth with intact biceps tendons who are not in pain, so it cannot be called a "pain generator".
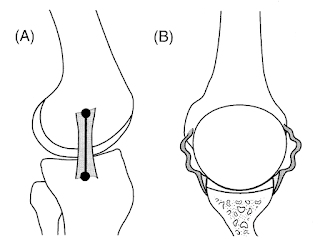
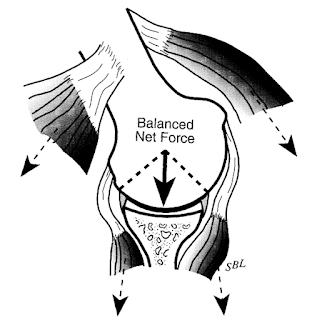
In the normal shoulder the (LHTB) provides a secure anchor for half of the biceps and stability for the shoulder - both through its contribution to concavity compression and also by the "monorail" mechanism in which the transverse humeral ligament and intertuberular groove glide along the biceps monorail providing increasing stability against anterior and posterior translation as the humerus is elevated as shown in this nice diagram by Steve Lippitt.
While Speed-s and Yergason's tests are often used to detect pathology of the LHTB, we have found that the saw test is more sensitive and specific. In this test the elbow is held at 90 degrees of flexion holding a weight as shown in the video below.
Out of respect for the stabilizing function of the long head tendon of the biceps we are biceps keepers rather than biceps killers when we perform shoulder arthroplasty. We will only sacrifice the biceps if it is seriously frayed or unstable in the groove.
In 50 years of doing shoulder arthroplasty, we've never had to take a patient back to the OR for postoperative biceps issues. There is one patient who had biceps symptoms when she played golf and a positive saw test. Her symptoms responded to a single injection of her biceps sheath.
We always appreciate feedback and commentary on the blog. Jed Kuhn, immediate past president of the American Shoulder and Elbow Surgeons and consummate educator, after reading the post gave us a 'biceps reading list', which is included here:
Throwing, the Shoulder, and Human Evolution
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).