These authors analyzed 265 reverse total shoulder replacements (RTSAs) to determine the influence of preoperative opioid use on clinical and radiographic outcomes at a minimum of 2 years follow-up.
71 patients were classified as preoperative opioid users because they had taken narcotic pain medication for a minimum of 3 months prior to surgery (the Centers for Disease Control definition).
193 patients were classified as opioid-naive at the time of surgery.
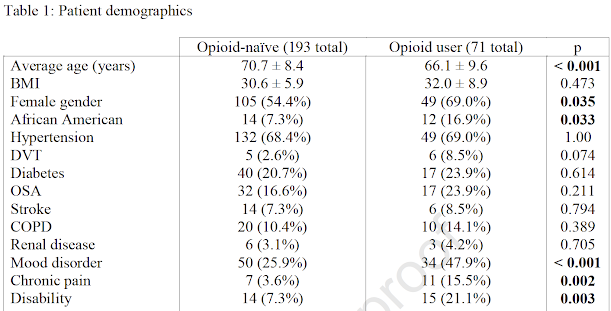
Opioid users were significantly younger, more likely to be female, more likely to be African-American and had significantly higher preoperative rates of mood disorders, chronic pain disorders, and disability status.
Postoperatively, opioid users had inferior VAS (2.59 vs 1.25), ASES scores (63.2 vs 75.2), active forward elevation, and internal and external rotational shoulder strength than opioid-naïve patients.
Both groups improved from baseline preoperatively to most recent follow-up in terms of functional outcomes and pain.
Opioid users had higher rates of complications (28.2% vs 17.1%) glenoid or humeral periprosthetic radiolucency (8.5% vs 2.1%), and subsequent revision arthroplasty (12.7% vs 4.7%).
Comment: This is an interesting study in that it found over one in four patients having RTSA to be using narcotics prior to surgery and that it suggests that opioid use may be a marker for psychosocial disorders that can increase the risk of poorer outcomes.
The unanswered questions are
(1) can these psychosocial disorders and opiod use be effectively modified prior to surgery so that outcomes are improved?
(2) how should the presence of opioid use change our indications for RTSA for patients who otherwise would be candidates for this procedure?
(3) if the decision is made to proceed with RTSA, how can the postoperative care for the opioid using patient be optimized?
(4) does dose and type of narcotic matter? Compare the patient who takes one oxycodone at night for sleep to the patient who is taking substantial doses of oxycontin, suboxone or MScontin?
We are grateful to the senior author of this paper for his thoughtful responses to these questions:
- can these psychosocial disorders and opiod use be effectively modified prior to surgery so that outcomes are improved?
We don’t really think so. Opioid use in our practice is typically “baked into the cake” due to a number of prior factors that are very difficult to undo prior to surgery. We use this information as a pre-operative education piece to let patients know they can make improvements after surgery, but not to the level that their peers may achieve (or that the patient may wish).
- how should the presence of opioid use change our indications for RTSA for patients who otherwise would be candidates for this procedure?
It’s a data point that we consider but does not by itself change indications. Again, we use this for patient education pre-operatively.
- if the decision is made to proceed with RTSA, how can the postoperative care for the opioid using patient be optimized?
In our state regulations only allow opioid medications to be given by one provider. So if a patient presents already taking opioids, we typically defer post-operative opioid management to that provider if possible. In some instances, that provider may wish for us to manage the opioids for up to 3 months post-operatively and we are amenable to that. Either way, we employ multimodal pain management (intraoperative periarticular injections, gabapentin, scheduled Tylenol, and muscle relaxers). If we are managing the opioids, we maintain the patient on their pre-operative dose and supplement with oxycodone 5-10mg per dose for breakthrough pain. As our data suggests however, these patients have a more difficult post-operative course and have more difficulty with pain control.
- does dose and type of narcotic matter? Compare the patient who takes one oxycodone at night for sleep to the patient who is taking substantial doses of oxycontin, suboxone or MScontin?
We have a previous study on opioid use prior to anatomic TSA which did find a dose-response relationship between opioid use and outcomes. While difficult to directly extrapolate to reverse arthroplasty, we suspect this relationship likely still holds. However, the data also suggests a discrete (yes-no) phenomenon where any amount of pre-operative opioid use is detrimental.
In our practice we assess each patient individually in partnership with a primary care physician who agrees to assist in addressing (1) the psychosocial issues and (2) assisting the patient in withdrawing from narcotics before surgery. If the patient cannot withdraw from narcotics before surgery, the primary care physician must agree to manage these medications after surgery. We emphasize that patients taking substantial narcotics prior to surgery cannot expect the same degree of pain relief as the person who is opioid naive.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
How you can support research in shoulder surgery Click on this link.
Here are some videos that are of shoulder interest