Outcomes of shoulder arthroplasty by year of index procedure: are we getting better?
These authors performed a retrospective analysis of 1899 patient-reported outcomes from their institution’s registry between 2008 and 2018 for anatomic (aTSA) and reverse (RTSA) shoulder arthroplasty. Of 2952 patients entered into the registry, 2 and/or 5 year followup data were available in 1899 (64%); over one-third of the patients did not have followup data.
The average preoperative to postoperative improvement in ASES score for patients reporting two-year followup did not change over time for either aTSA or RTSA
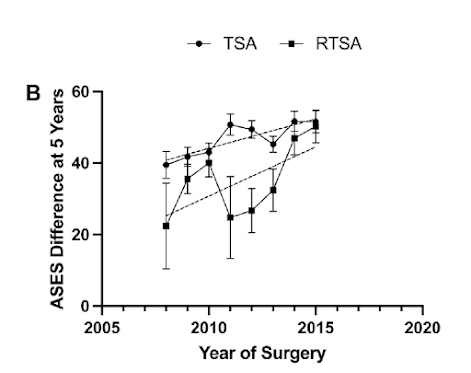
The average preoperative to postoperative improvement in ASES score for patients reporting five-year followup was higher for more recently performed surgeries.
Note in both of the graphs above that the improvement in ASES scores was consistently greater for aTSA than for the more expensive RTSA. Thus the value (benefit/cost) was greater for aTSA.
ASES scores were associated with patient sex, American Society of Anesthesiologists classification, rotator cuff status, primary diagnosis, Walch classification, and revision procedures. Specifically included patients from more recent surgeries were more likely to have a diagnosis of primary osteoarthritis. This was particularly the case for patients having rTSA.
Over the duration of this study there were decreases in the rates of aTSA patients having rheumatoid arthritis, avascular necrosis, cuff tear arthropathy, torn rotator cuff or‘‘other’’ diagnoses relative to OA over time.
There were decreases in the rates of RTSA patients with acute fracture, old trauma, cuff tear arthropathy, instability, infection, and ‘‘other’’ diagnoses.
Therefore for both procedures, the percentage of the straightforward diagnosis increased while that of the more complex diagnoses decreased.
Comment: Interestingly the 50 point improvement in ASES scores for the most recently performed anatomic shoulder arthroplasties in this study was similar to the improvement reported in a recent publication Assessing the Value to the Patient of New Technologies in Anatomic Total Shoulder Arthroplasty across 20 years:
In that publication, the reported amount improvement in ASES scores after aTSA did not change over two decades (see chart above).
The results of Outcomes of shoulder arthroplasty by year of index procedure: are we getting better?suggest that the improved results these surgeons observed for more recently performed surgeries may be attributed in large part to a shift in indications for shoulder arthroplasty away from more complex diagnoses in favor of the more straightforward diagnosis of osteoarthritis.
This paper did not assess the value of new implants or technologies, such as preoperative 3D CT planning, in improving the outcome of shoulder arthroplasty. In their discussion they point out that patients receiving newer implant designs do not always achieve better clinical outcomes (see Is there evidence that the outcomes of primary anatomic and reverse shoulder arthroplasty are getting better?) In "Does an increase in modularity improve the outcomes of total shoulder replacement? Comparison across design generations." the authors examined three different generations of implants for total shoulder arthroplasty, determining that second and third generations of glenoid components were at a higher risk of failure when compared with first generation implants.
Since the date of surgery is usually not a modifiable predictor of the result of shoulder arthroplasty, we need to continue to evaluate the importance of procedure selection and surgical technique in optimizing arthroplasty outcomes for patients with different diagnoses and personal characteristics.
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
How you can support research in shoulder surgery Click on this link.
Here are some videos that are of shoulder interest