Arthritis of the shoulder with an intact rotator cuff has been reliably managed with an anatomic total shoulder arthroplasty (TSA) for decades. However, the use of reverse total shoulder (RSA) to treat this diagnosis has recently increased dramatically to the point where fully one third of reverses are being performed for straightforward arthritis (see Increasing incidence of primary reverse and anatomic total shoulder arthroplasty in the United States). This shift may be a result of the "reverse for everything" approach espoused by some surgeons leading to the use of the reverse in almost two thirds of all shoulder arthroplasties.
While there is a concern about rotator cuff failure and glenoid component loosening 10 - 15 years after anatomic arthroplasty, there is also a concern about dislocation and acromial/scapular spine fractures after reverse total shoulder arthroplasty. In that these complications may not lead to repeat surgery, revision and "survival" rates may not accurately reflect the complication rate.
The value of an arthroplasty is defined as the benefit realized by the patient divided by the costs associated with the procedure. In that the cost of a reverse is substantially greater than that of an anatomic arthroplasty, the patient benefit must be substantially greater for RSA to achieve the same value as for TSA.
The authors of Outcomes After Anatomic and Reverse Shoulder Arthroplasty for the Treatment of Glenohumeral Osteoarthritis: A Propensity Score-Matched Analysis performed a retrospective matched-cohort study of patients with a minimum of 2 years of follow-up after a TSA and RSA for the treatment of primary osteoarthritis by a high volume shoulder arthroplasty surgeon.
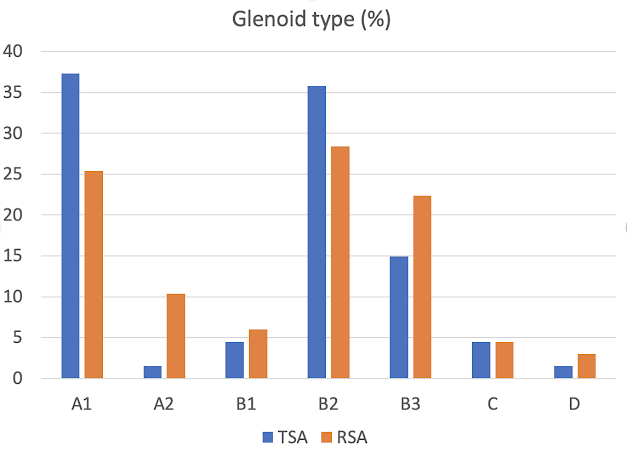
One hundred and thirty-four patients (67 patients per group) were included, each with an intact rotator cuff by MRI. The reasons for selecting RSA versus TSA are not described. Patients were propensity score-matched by age, sex, body mass index (BMI), preoperative American Shoulder and Elbow Surgeons (ASES) score, preoperative active forward elevation, and - importantly - for Walch glenoid morphology.
Notably no augmented glenoid components were used.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interestShoulder arthritis - what you need to know (see this link).How to x-ray the shoulder (see this link).The ream and run procedure (see this link).The total shoulder arthroplasty (see this link).The cuff tear arthropathy arthroplasty (see this link).The reverse total shoulder arthroplasty (see this link).The smooth and move procedure for irreparable rotator cuff tears (see this link).Shoulder rehabilitation exercises (see this link).
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/