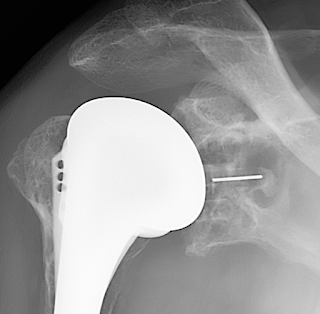
Glenoid component failure remains a most important cause of failure after total shoulder arthroplasty (see Glenoid component failure in total shoulder arthroplasty). Glenoid component failure may be related to
(1) poor surgical technique, such as inadequate seating of the component (see The radiographic evaluation of keeled and pegged glenoid component insertion), the use of back-side cement to compensate for inadequate glenoid bone preparation
(2) inferior polyethylene leading to wear and particulate debris (see this link),
(3) metal backed components (see Metal-Backed Glenoid Components Have a Higher Rate of Failure and Fail by Different Modes in Comparison with All-Polyethylene Components: A Systematic Review
(4) poor humeral component placement
(5) instability or cuff failure giving rise to rocking horse loosening from eccentric loading of the glenoid component (see Glenoid loosening in total shoulder arthroplasty. Association with rotator cuff deficiency)
and (6) infection (see Loose glenoid components in revision shoulder arthroplasty: is there an association with positive cultures?)
Glenoid component failure may become clinically evident years after the index procedure as in this case that came to revision 24 years after the index procedure.
Total Shoulder Arthroplasty: Can it Work?
However, this approach does not allow for revision of the humeral head component to compensate for the loss of the glenoid component, which can be accomplished at open revision as shown below.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interestShoulder arthritis - what you need to know (see this link).How to x-ray the shoulder (see this link).The ream and run procedure (see this link).The total shoulder arthroplasty (see this link).The cuff tear arthropathy arthroplasty (see this link).The reverse total shoulder arthroplasty (see this link).The smooth and move procedure for irreparable rotator cuff tears (see this link).Shoulder rehabilitation exercises (see this link).
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/