As pointed out by the authors of Effect of obesity on short and long-term complications of shoulder arthroplasty, the number and percent of obese patients having shoulder arthroplasty in the United States is steadily increasing each year.
They sought to evaluate postoperative medical and surgical complications in patients with obesity undergoing anatomic and reverse total shoulder arthroplasty using a national database.
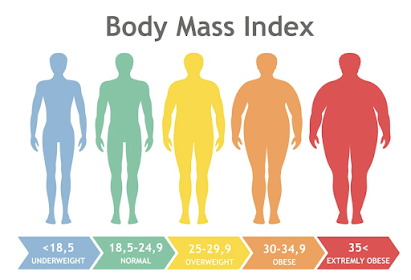
A matched cohort analysis demonstrated higher odds of readmission, deep vein thrombosis/pulmonary embolism, superficial infection, and prosthetic joint infection at 90 days postoperatively in the obesity group. Medical complications and infection after total shoulder arthroplasty were greater in obese patients even when matching for medical comorbidities, age, and sex. The rates of complication increased with higher body mass index (BMI).
While there was an increased risk of mechanical complications and revision surgery at 2 years in the obesity group, this effect was not significant when matched to non-obese patients with similar comorbidities.
The odds of readmission, DVT/PE, superficial infection, acute kidney injury and periprosthetic infection were doubled in severely obese patients.
Comment: This study shows yet another serious health problem associated with the obesity epidemic. It prompts us to ask several questions:
(1) Is obesity truly a "modifiable" risk factor?
(2) Is there evidence that weight loss (i.e. from diet, bariatric surgery, medications) reduces the risks of surgery. Might abrupt weight loss actually increase surgical risk?
(3) In that shoulder arthroplasty is usually an elective procedure, how should these data affect our indications for this surgery?
(4) How does obesity affect the clinical outcomes of shoulder arthroplasty?
The authors of Effects of Obesity on Clinical and Functional Outcomes Following Anatomic and Reverse Total Shoulder Arthroplasty addressed point #4.
They identified 1520 patients having primary anatomic (aTSA) arthroplasty and 2054 patients having primary reverse total shoulder arthroplasty with a minimum follow-up of 2 years (mean 5 years). All patients received the same platform shoulder prosthesis.
Patients were stratified according implant type (anatomic or reverse), and further stratification was based on patient BMI, with obese patients having a BMI ≥ 30 kg/m2 and non-obese patients with a BMI <30 kg/m2.
41% of aTSA and 35% of rTSA were obese.
Obese patients in both groups reported higher preoperative and postoperative visual analog scale (VAS) pain scores (i.e. more pain) and less preoperative and postoperative ROM compared to non-obese patients.
Compared to non-obese patients, obese patients receiving an aTSA reported significantly worse postoperative SST, Constant, ASES, UCLA, and SPADI scores compared to non-obese patients, and those receiving rTSA reported significantly worse ASES and SPADI scores. However, these differences did not exceed the minimal clinical important difference (MCID) or substantial benefit (SCB) criteria.
 Statistically significant differences between obese and non-obese groups were not found to be clinically relevant given that the differences between the two groups with regards to VAS pain scores, ROM, and functional outcome scores did not exceed the MCID and SCB criteria in both the aTSA and rTSA groups.
Statistically significant differences between obese and non-obese groups were not found to be clinically relevant given that the differences between the two groups with regards to VAS pain scores, ROM, and functional outcome scores did not exceed the MCID and SCB criteria in both the aTSA and rTSA groups.
Radiographic analysis 23 showed that in rTSA, obese patients had significantly less postoperative scapular notching and a lower scapular notching grade when compared to non-obese patients (P<0.05).
Obese patients had more comorbidities, greater intraoperative blood loss.
Overall complication rates were similar between obese and non-obese groups for both aTSA (7.6% vs. 8.4%; p = 0.57) and rTSA (3.4% vs. 3.9%), including rotator cuff tears, instability, infection, component loosening or failure, dislocation, liner dissociation, stress fracture, neurological complaints, and pain. Revision rates secondary to these complications were also similar between obese and non-obese groups for both aTSA (5.1% vs 5.9%) and rTSA (2.1% vs. 1.7%).
One of the more interesting findings in this study was that obesity seemed to protect patients against scapular notching and a higher notching grade. It seems possible that obesity limited adduction of the arm, reducing the contact between the medial edge of the humeral cup and the lateral scapular neck.
It is of interest to review some of the previous posts on the topic:
Is it safe to operate on patients with obesity?
Reverse total shoulder in obese patients - the 4 Ps
Malnutrition and arthroplasty outcomes
Shoulder arthroplasty - malnutrition increases risk
Adverse outcomes from total shoulder arthroplasty - the role of malnutrition
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interestShoulder arthritis - what you need to know (see this link).How to x-ray the shoulder (see this link).The ream and run procedure (see this link).The total shoulder arthroplasty (see this link).The cuff tear arthropathy arthroplasty (see this link).The reverse total shoulder arthroplasty (see this link).The smooth and move procedure for irreparable rotator cuff tears (see this link).
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Shoulder rehabilitation exercises (see this link).