Preoperative joint fluid aspirates are often sent for bacterial culture in the hope of determining the presence and type of organisms in failed shoulder arthroplasties.
The authors of What is the concordance rate of preoperative synovial fluid aspiration and intraoperative biopsy in detecting periprosthetic joint infection of the shoulder? sought to evaluate the utility of preoperative culture data for early pathogen identification for shoulder PJI.
Their diagnosis of PJI was determined according to the older version of Musculoskeletal Infection Society criteria established in 2014. They included only patients meeting these criteria who underwent revision for shoulder PJI with both preoperative synovial fluid culture and intraoperative tissue culture data. Notably, patients with "dry" taps were excluded - the number of cases excluded for this reason are not disclosed.
50 patients were included. Antibiotics were held 2 weeks before the aspiration. Intraoperative cultures were obtained before the administration of perioperative antibiotics. Five to 8 tissue samples were collected from multiple surgical sites.
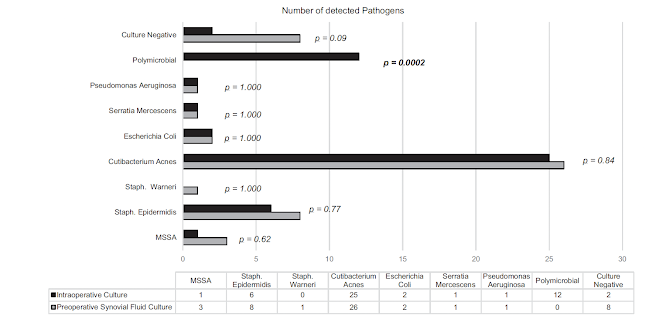
42 (84%) preoperative synovial fluid aspirations were monomicrobial, and 8 (16%) were culture negative. Six of the 8 shoulder PJIs (75%) with negative preoperative cultures were found to have positive intraoperative cultures.
36 (72%) of the intraoperative cultures were monomicrobial, 2 (4%) were culture negative and, notably 12 (24%) were polymicrobial - these were not identified on preoperative fluid aspirate cultures.
Cutibacterium was recovered on intraoperative cultures of 50% of the cases (25/50). 82% of the cases had low virulence organisms.

High virulence pathogen (methicillin sensitive staphylococcus and gram negative bacteria) infections were detected on fluid aspirates in all 7 cases.
The sensitivity and specificity of preoperartive fluid cultures for Cutibacterium were 0.76 and 0.72. Gram-negative pathogens demonstrated the highest sensitivity and specificity, whereas polymicrobial infections exhibited the lowest sensitivity and positive predictive value.

The "concordant" group consisted of patients who had the same bacteria in both groups. For polymicrobial samples, the same bacteria needed to be present in both the preoperative and intraoperative culture to be included in the concordant group. The discordant group had at least 1 different pathogen.
Concordance between preoperative aspiration and intraoperative tissue culture was identified in only 28 of 50 patients (56%) with a discordance rate of 44%.
Preoperative cultures positive for Gram-positive species and those positive for Cutibacterium were more likely to be concordant than discordant.
Comment: This study found that cultures of preoperative fluid aspirations often failed to predict the complete intraoperative microbiology of shoulders meeting criteria for periprosthetic infection.
Perhaps the more important question is "what is the utility of preoperative joint fluid cultures in all patients requiring shoulder arthroplasty revision?" In other words, how might these cultures change treatment? It seems that fluid aspirate cultures are most useful in the preoperative identification of high virulence organisms. The presence of high virulence organisms is suggested by systemic signs of illness combined with shoulder joint warmth, swelling and tenderness - an "obvious" infection. In such cases aspiration to identify organisms such as E. Coli, Pseudomonas, MRSA, MSSA, and Seratia is likely to be of value in planning surgery and postoperative antibiotics.
By contrast, the role of aspirate cultures for shoulders that have no obvious signs of infection is less clear. Often attempted aspiration in such cases yield no fluid - a "dry" tap. In other cases, as shown in this study, the aspirate may fail to reveal the causative organism (which is often Cutibacterium).
The authors of another recent article, The role of synovial fluid aspiration in shoulder joint infections, found that preoperative aspiration failed to yield a sufficient volume for culture in 11 of 35 cases. Even in the cases of sufficient fluid volume, they concluded that preoperative aspiration is likely to miss Cutibacterium and coagulase negative staphylococcus. However, they recommended considering aspiration as a means of possible germ identification. They felt that empiric antibiotic therapy should cover Cutibacterium and coagulase negative staphylococcus even if aspiration showed negative microbiological cultures.
One way to look at this not-uncommon clinical challenge is that a dry or culture negative tap does not provide assurance of lack of joint infection. On the other hand, a positive preoperative culture of joint fluid raises the chances of having positive intraoperative cultures. Other risk factors for PJI with low virulence organisms include the delayed "stealth"onset of unexplained pain and stiffness after an initially successful rehabilitation (a "honeymoon period"), young age, male sex, high levels of Cutibaterium on the unprepared skin of the shoulder, prior surgery, high levels of serum testosterone, and humeral component loosening. These findings may prompt consideration of a single stage prosthetic exchange followed by vigorous antibiotic therapy.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).

