At four years after surgery, the right stemless component (below left) shows localized absence of bone beneath the inferior aspect of the humeral head (green arrow).
At four years after surgery, the left short stemmed component (below right) shows reduced bone density proximal to the diaphysis into which the component has been tightly inserted (black arrows). The red arrows show the localized osteopenia of the lateral humerus while the yellow arrows show the absence of bone medially.

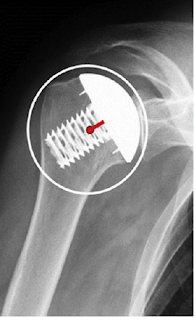
As pointed out in a prior post, with stemmed implants loads applied to the humeral head are distributed by the stem to the humeral diaphysis. However, with the stemless humeral arthroplasty, loads applied to the prosthetic humeral head are distributed to the humeral metaphysis (blue rectangle), bypassing the humeral cortex unless there is contact between the head and humeral neck cut (red arrows). The degree of cortical loading is a function of implant design and surgical technique.
In this post we'll take a closer look at what's been published about stress shielding and adaptive changes after stemless humeral arthroplasty. There's a lot here so you may want to skip to the Comment at the bottom to see a summary.
Computer model studies
The effect of stemless humeral component fixation feature design on bone stress and strain response: a finite element analysis analyzed the effect of several different humeral component fixation design features

The bone adaptation process was evaluated by comparing differences in bone density between the implanted models and the intact model of the humerus.
The Eclipse-based design was associated with the largest bone mass loss, whereas the SMR based design caused the least. When contact was simulated between the resected bone surface and the humeral head components of the SMR-, Simpliciti-, and Sidus-based designs and, bone resorption increased.
Notably, the clinical papers reviewed below show a wide spread in assessment methods and in the reported rates of stress shielding in the humerus after stemless arthroplasty.
There was no reported evidence of migration, subsidence, osteolysis, or loosening of the humeral components.
The authors of Screw fixation in stemless shoulder arthroplasty for the treatment of primary osteoarthritis leads to less osteolysis when compared to impaction fixation compared their results with the Eclipse Shoulder Prosthesis
they found no osteolysis of the medial calcar at a mean of 42 months in 18 patients having the Eclipse; however with the Sidus, osteolysis of the medial calcar was present in seven of the 21 patients at a mean of 36 months after surgery (see above).
Results for the Eclipse implant were reported in Midterm results of stemless shoulder arthroplasty: a prospective study for 78 patients at a minimum follow-up of 5 years. Bone mineral density was reduced in 34.9% of the older population.
Nine-year outcome after anatomic stemless shoulder prosthesis: clinical and radiologic results presented results for 49 patients receiving the Eclipse shoulder prosthesis at mean of 9 years. Localized lowering of bone density was seen in 29% of the patients.
Radiological changes do not influence clinical mid-term outcome in stemlesshumeral head replacements with hollow screw fixation: a prospective radiological and clinical evaluation used the Eclipse shoulder prosthesis 73 patients, 37% of which had localized bone loss.
Survival of stemless humeral head replacement in anatomic shoulder arthroplasty: a prospective study reported outcomes for 75 patients having the Eclipse shoulder prosthesis with a mean followup of 126 months. Stress shielding around the humeral component was not detected.
Mid-term results with an anatomic stemless shoulder prosthesis in patients with primary osteoarthritis evaluated 38 patients at an average of 37 months after insertion of a TESS stemless shoulder prosthesis. No signs of stress shielding were noted.
The authors of Short-term radiographic analysis of a stemless humeral component for anatomic total shoulder arthroplasty reported the two year radiographic outcomes for 54 patients receiving the Equinoxe Stemless. Stress shielding was observed in 4 patients (7%) with the medial calcar being the most common location of stress shielding. Three of the 4 patients had evidence of partial resorption while 1 patient (25%) had evidence of complete resorption.
Proximal humeral bone loss in stemless shoulder arthroplasty: potential factors influencing bone loss and a new classification system. found that women patients were more likely to experience bone loss after stemless arthroplasty with the Affinis Short Stemless Anatomic Shoulder Prosthesis. Shown below are anteroposterior radiographs demonstrate bone loss grades at the proximal humerus. Grade 0: no bone loss, grade I: bone loss with rounding off of the medial calcar, grade II: bone loss with the corner of the metallic fin at the medial calcar exposed, and grade III: bone loss up to the central stem at the medial calcar. Arrows indicate areas of bone loss.
The SPECT/CT data suggested that the primary osseointegration of the stemless shoulder prosthesis was almost completed 3 months after implantation.
Reliability of stemless shoulder arthroplasty in rheumatoid arthritis:observation of early lysis around the humeral component compared outcomes for the Affinis Short in 35 patients with RA to 35 patients with osteoarthritis.The proportion of progressive proximal humeral bone loss after TSA was 33% in the RA group and 13% in the control group. Two examples of severe bone loss are shown below.
Impact of humeral stem length on calcar resorption in anatomic total shoulder arthroplasty was a retrospective review of TSA patients treated with three different-length humeral implants (canal-sparing, short, and standard-length designs). Patients were matched 1:1:1 based on both gender and age (±4 years), resulting in 40 patients per cohort. The canal-sparing implant was the Enovis CS Edge. At 3 months, calcar resorption was observed in 20% of the canal sparing cohort, while the short and standard designs demonstrated resorption in 55% and 52.5%, respectively. At 12 months, calcar resorption was seen in 65% of the canal-sparing design, while both the short and standard designs had a 77.5% rate of resorption. The severity of calcar resorption for the canal-sparing cohort was significantly lower at all time points when compared to the short stem.
Follow on twitter: https://twitter.com/RickMatsen or https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).