While many investigations study glenohumeral and scapulothoracic relations with the arm at the side or in abduction, most of the activities important to patients are performed with the arm elevated in a forward direction.
In this position the humeral head is centered by concavity compression: the net force on the humeral head compresses it into the glenoid concavity.
If the joint reaction force does not pass through the glenoid concavity, the glenohumeral joint is unstable.
Because the glenoid concavity is less wide in the anterior and posterior directions than in the superior and inferior directions,
the stability ratios are less in the anterior and posterior directions.
An important feature of the shoulder is that, in contrast to the hip joint, the socket can be positioned to optimize stability.

So with the scapula in the position on the image below left, the force applied to the glenohumeral joint does not pass through the glenoid so that the stability of the articulation must be supported by the posterior soft tissues. By contrast the image below right shows that the scapula is positioned so that the glenoid fossa supports the humeral force.
From the foregoing we can see that during ordinary functional activities, the posterior articular cartilage is disproportionately at risk for wear and the posterior soft tissues are at risk for failure (e.g. posterior labral tear and/or stretching of the posterior capsule). Thus there is a potential for a vicious cycle in which compromise of the posterior supporting structures leads to more instability when the arm is in a position of function, which leads to greater posterior glenoid wear and more failure of the posterior soft tissues.
An additional element in this vicious cycle may be progressive anterior capsular tightness leading to posterior humeral head translation and increased pressure on the posterior glenoid when external rotation is attempted.
Unfortunately, two of the most commonly used methods for imaging the glenohumeral relationship (MRI and CT) are obtained with the arm at the side, rather than in a position of function.
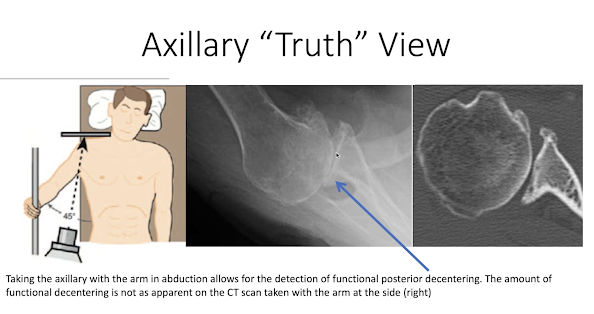
Fortunately, functional instability can be imaged by the axillary "truth" view, in which the arm is elevated into the position of function.
Below are three examples of posterior decentering shown on the axillary "truth" view in shoulders with minimal arthritic changes.
The authors of Walch B0 glenoid: pre-osteoarthritic posterior subluxation of the humeral head refer to pre-osteoarthritic posterior subluxation of the humeral head as a Walch B-zero (B0) glenoid. They suggest that the Walch B0 glenoid is a pathologic condition that is initially dynamic and that eventually evolves into a static condition with posterior erosion of the glenoid.
Our experience is that the axillary truth view can reveal dynamic posterior decentering of the humeral head when the arm is in a functional position of forward elevation before substantial arthritic changes have taken place and before the decentering becomes evident on CT scans and MRI images obtained with the arm at the patient's side.
Early identification of functional decentering can help the surgeon explain the patient's symptoms and discuss early interventions that may slow the progression of symptoms. Such interventions may include activity modification (e.g avoiding heavy bench presses), scapular positioning training (e.g. learning scapular protraction to keep the humeral head supported by the glenoid),
and external rotation strengthening (to help keep the net humeral force centered in the glenoid).
It is also possible that a release of the tight anterior capsule may mitigate the obligate posterior translation that can result from it.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link Shoulder rehabilitation exercises (see this link).