Anatomic total shoulder arthroplasty reliably provides long term comfort and function for patients with osteoarthritis and an intact rotator cuff, even in patients with deficiencies in glenoid bone (see
Anatomic Total Shoulder Arthroplasty with All-Polyethylene Glenoid Component for Primary Osteoarthritis with Glenoid Deficiencies). While some surgeons attempt to "correct" the patient's glenoid version, others "accept" it (see
Glenoid Version, Acceptors and Correctors). It either case, one of the most important technical goals of anatomic total shoulder arthroplasty is excellent seating of the glenoid component (see
Edge displacement and deformation of glenoid components in response to eccentric loading. The effect of preparation of the glenoid bone).
Good seating is achieved by reaming the glenoid bone to a single concavity
that matches the backside of the glenoid component
so that no cement is placed between the bone and the backside of the prosthesis to fill in the gaps,
backside cement indicates poor seating and risks cement failure
below is an example of a well-seated glenoid component. The only cement visible is in the peg holes.
To further investigate the technical factors associated with anatomic total shoulder (aTSA) outcomes, the authors of
Anatomic total shoulder arthroplasty for posteriorly eccentric and concentric osteoarthritis: a comparison at a minimum 5-year follow-up evaluated 210 patients at a minimum of five years after aTSAs performed with conservative glenoid reaming with no attempt at version correction.
Preoperatively, 98 (47%) had posteriorly decentered humeral heads and 108 (51%) had centered humeral heads. There were 77 shoulders with Walch type A glenoids and 122 with Walch type B glenoids.
At a mean 8-year follow-up, the final SST score, change in SST score, and percentage of maximal improvement were not correlated with preoperative or postoperative humeral head centering, Walch classification, or glenoid version.
Two patients (1%) underwent open reoperations during the study period.
In patients with Walch B1 and B2 glenoids (n = 110), there were no differences in outcome measures between patients that had postoperative retroversion of more or less than 15°.
Although 15 of 51 patients (29%) with minimum 5-year radiographs had glenoid radioluciences, these radiographic findings were not associated with inferior clinical outcomes.
On multivariable analysis, glenoid component radiolucencies were most strongly associated with incomplete component seating.
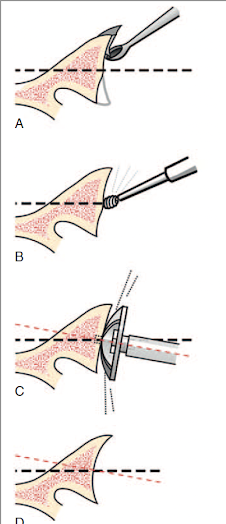
Careful preparation of the glenoid bone.
From the authors of Edge displacement and deformation of glenoid components in response to eccentric loading. The effect of preparation of the glenoid bone we learn that the wobble and warp of the polyethylene component is minimized by spherically reaming the bone to precisely match the back of the component.
Glenoid bone stock is preserved by reaming only enough to create a single concavity, rather than trying to "correct" glenoid version.
The adequacy of glenoid reaming can be evaluated by using a pegless trial with the same backside curvature as the actual component and assuring that there is no rocking with eccentric loading. The goal is complete congruency.
Assuring optimal seating and cementing of the component.
From the authors of The radiographic evaluation of keeled and pegged glenoid component insertion we learn that poor seating and poor cement technique contribute to poor fixation as evidenced by radiolucent lines on the immediate postoperative x-rays.
Poor seating is evidenced by the presence of cement between the glenoid bone and the backside of the component.
Good seating is indicated by the absence of cement between the component and bone (below top), rather than using cement as putty in an attempt to compensate for inadequate reaming.
A thin layer of cement between the bone and component is brittle and subject to cracking, displacement and loss of support for the glenoid implant.
Optimal cementing is reflected by the absence of radiolucent lines on postoperative radiographs.
We have learned that this can be achieved by drying each fixation hole with a CO2 spray
Immediately before pressurizing the cement into the hole
Comment: The survivorship of cemented, pegged, all-polyethylene glenoid components has yet to be surpassed by other types of glenoid implants (see Total shoulder replacement stems in osteoarthritis-short, long, or reverse? An analysis of the impact of crosslinked polyethylene). Attention to the details of bone-preserving bone preparation, complete seating of the component and modern cement technique may further improve the clinical outcomes of anatomic total shoulder arthroplasty. Our technique for this procedure is shown in this link.