On 22 October 1895, there was a particularly spectacular railway accident at the Gare de l'Ouest in Paris. The No.56 train arriving from Grandville hurtled into the station at a speed of 40 to 60 kilometres an hour, and, unable to stop, plowed through the buffers at the end of the platform. Its engine crashed through the façade of the station building, and fell down on to the Place de Rennes.
Hopefully the responsible railway system, Chemins de fer de l'Ouest, learned more from studying this failure than from studying all their on time, safe arrivals.
The May 26, 2025 post, "Do higher case volumes make us safer and more effective surgeons?", pointed out that it is not the number of cases we do that make us better, but rather the study of our failures that provide a path to improvement. This post also pointed out that the surgeon performing the procedure is, in many instances, the most important determinant of the outcome: the surgeon is the method.
The authors reported excellent average outcomes for 128 consecutive anatomic total shoulder arthroplasty (aTSA) using non-augmented glenoid implants and short humeral stems for glenohumeral arthritis with an intact rotator cuff. In spite of the average success, they sought to identify factors associated with adverse outcomes.
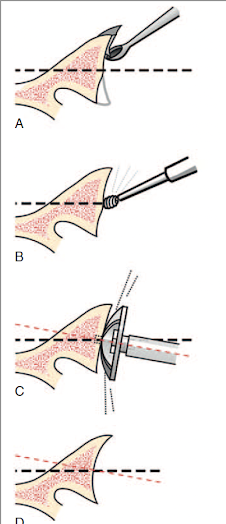
The surgeon's technique included minimal glenoid reaming to achieve >90% backside contact of a pegged, all polyethylene standard glenoid implant, inserted with minimal cement. The surgeon used a subscapularis peel which was repaired after insertion of the components using 6 to10 high-strength #2 braided sutures passed through transosseous drill holes. After the implants were placed, the subscapularis tendon was closed with these sutures and with closure of the distal rotator cuff interval with additional braided sutures to reinforce the repair.
104 of the 128 aTSAs were available for evaluation at minimum 2 years follow-up (range 2-5.6 years) (see the challenge of longer term followup). In comparison to many published reports, this represents a high percent followup. The authors included information on the remaining 24 - a few had passed on or became invalid, a few were revised and only a dozen or so could not be tracked. In clinical studies the denominator counts big and the reasons for loss to followup are important.
As stated in A Study in Hospital Efficiency (Codman, E.A. 1917). "All patients should be followed long enough to determine whether or not the treatment has been successful, and to ask 'if not, why not?'".
Overall, mean ASES scores improved from 41 to 89, SST from 4.5 to 10, and VAS-pain from 5.5 to 0.7. [Note that these average postoperative scores are within the minimal clinically important differences of perfect scores. Thus it would be statistically impossible for any change in implant or technique (for example, routine use of preoperative 3D CT planning) to make a clinically significant improvement in the average outcomes.]
Fifty-nine patients had preoperative posterior glenoid wear patterns (Walch B2 or B3) and 47 had concentric or minimal glenoid wear (Walch A1, A2, or B1). The presence of posterior glenoid wear was not found to influence any outcome score
There were three modes of failure identified by the authors
(1) Subscapularis failure: 5 patients underwent revision to reverse shoulder arthroplasty for subscapularis insufficiency and one underwent open subscapularis repair with graft augmentation following traumatic injury. Three of the subscapularis tears arose because of trauma and/or patient reported noncompliance with postoperative immobilization or restrictions. All but one of the subscapularis failures reported here occurred within the first 12 months postoperatively. None of the patients with subscapularis failure requiring surgery had undergone prior open capsulorrhaphy or subscapularis repair
(2) ASES score <70: Ten patients had a final ASES score < 70, which was associated with a history of previous surgery (overall, twenty-four shoulders had undergone previous surgery).
(3) Glenoid osteolysis: 10 patients (13%) had radiographs demonstrating glenoid osteolysis (defined as "radiolucency extending at least two mm from the center of peripheral pegs"). Glenoid osteolysis was not found to be associated with preoperative posterior glenoid erosion. The presence of glenoid osteolysis was not found to have an adverse effect on clinical outcome with the period of followup in this study.
Comment: These authors report overall excellent results with their surgical technique. They have also defined three adverse outcomes that merit further study so that they and we can learn to avoid them.
Subscapularis failure: It would be of interest to know the rehabilitation program used by the surgeon. I am using a "slow roll" approach to range of motion exercises during the first six weeks and spend time cautioning the patient about falls and about avoiding external rotation stretching and active internal rotation during this period. Perhaps this surgeon does the same.
Prior surgery: It's a fact that young patients with arthritis commonly have had prior surgery. While the patient's history is not modifiable, we should try to learn if these patients have particular issues that could be addressed at surgery, such as (a) stiffness that might drive consideration of more aggressive soft tissue releases or smaller components or (b) difficulty in centering the humeral head on the glenoid that may drive use of eccentric humeral head components.
This is a fine example of an individual surgeon study that has identified three adverse outcomes from anatomic arthroplasty. While it is unlikely that modifications in the surgical technique will lead to clinically significant improvement in the average outcome scores (because the average scores reported are so good), it is possible that additional study of patients with these failure modes may show us how to lower their frequency.
The first step is to define the problems.
Fish with a problem
Montake Fill, Seattle June 2019
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link)
Shoulder rehabilitation exercises (see this link).