A major component of the success of reverse total shoulder arthroplasty is the position and orientation of the base plate on the glenoid bone. While many different planning systems are available, the challenge is transferring the plan to the patient without relying on expensive and time-consuming approaches, such patient specific instrumentation or augmented reality.
Our usual target is to have the inferior edge of the baseplate at the inferior aspect of the reamed glenoid and tilted inferiorly with the central screw or peg inclined so that it is parallel to the floor of the supraspinous fossa.
For routine cases, we plan for rTSA using plain x-rays obtained in the plane of the scapula (Grashey view). The scaled image is uploaded to the universally available PACS (Picture Archiving and Communication System). PACS tools are used to find the location of insertion point and the inclination of the drill for the central screw or post. These scaled measurements are then used to position and orient the drill on the patient's glenoid in the operating room. This generic approach does not encourage the surgeon to select implants from any particular company.
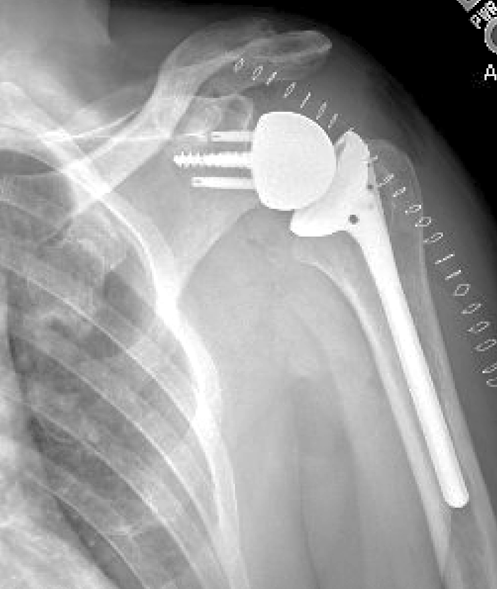
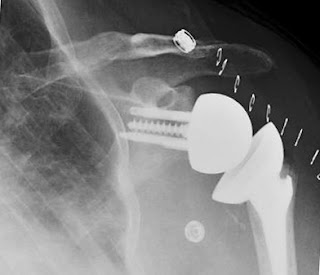
Here's an example: a 70 year old man with a massive irreparable cuff tear and pseudo paralysis.
On the PACS screen a line segment (yellow) with a length equal to the radius of the base plate is drawn perpendicular to the floor of the supraspinatus fossa (red line) from the glenoid articular surface to the glenoid neck. The upper end of this line is the insertion point (yellow dot)
Favard et al have described four types of glenoid pathoanatomy in cuff tear arthropathy.
For some cases, such as types E1 and E3, this planning approach may indicate that excessive reaming of inferior glenoid bone would be necessary to achieve the desired baseplate position and orientation. In such cases superior bone grafting or an augmented baseplate may be called for.
While more sophisticated proprietary systems can be used for more complex pathoanatomy, this generic approach can be effective for a large percentage of rTSA cases.
We use a similar plain films/PACS approach to planning a stemless anatomic arthroplasty - see this link.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link)
Shoulder rehabilitation exercises (see this link).