Acromial stress fractures and scapular spine stress fractures are related primarily to unmodifiable patient risk factors: (1) poor bone density (osteoporosis, female sex, older age, and inflammatory arthritis) and (2) diagnoses of rotator cuff deficiency (cuff tear arthropathy and massive rotator cuff tear). These factors need to be identified preoperatively and discussed with the patient with respect to the decision to proceed with RSA, the postoperative progression of rehabilitation and monitoring for unexpected pain and loss of function, as well the consideration of more conservative surgical options for appropriately selected patients at risk (see Managing rotator cuff tear arthropathy: a role for cuff tear arthropathy hemiarthroplasty as well as reverse total shoulder arthroplasty).
Although patient factors are the primary determinant of the risk of ASF and SSF, implant selection and positioning are less important but modifiable risk factors for the surgeon to consider. Notably the important measures of the final reconstructed geometry are (1) the location of the center of rotation with respect to the scapula and (2) the location of the proximal humerus in relation to the scapula (not whether the implant is “onlay or inlay” or how the implants are classified (GM/HL, GM/HM, GL/HL, GL/HL)).
These surgeon-controlled variables need to be considered not only with respect to their effect on the risk of stress fractures but also with respect to their effect on patient comfort and function. For example, increased glenoid lateralization appears to be associated with a greater risk of ASFs, but it also is associated with improved rotation and lower rates of scapular notching and impingement. As another example, increased humeral lateralization appears to be associated with lower risk of stress fractures, but may also give rise to an increased risk of unwanted contact between the abducted arm and the acromion.
Additional elements deserve consideration.
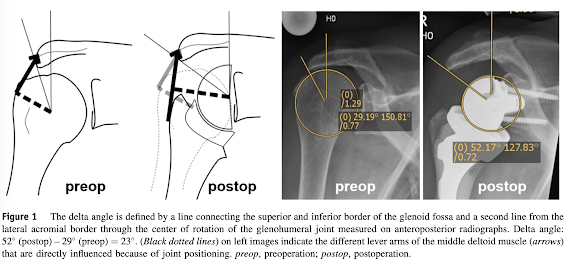
(1) Are we using the best method for determining the location of the center of rotation with respect to the scapula and the location of the proximal humerus in relation to the scapula (see figure above)? For example, the use of angles, such as the "lateralization shoulder angle" (LSA) and the "distalization shoulder angle" (DSA) to characterize linear measures of lateralization and distalization may be suboptimal for documenting the proximal/distal and medial/lateral position of the center of rotation and the proximal humerus.
(2) Should we be focusing only on the postoperative geometrical relationships, or should we also be paying attention to the preoperative to postoperative changes in these relationships, recognizing that the magnitude and direction of these changes may also influence the loads on the acromion and scapular spine? See A method for documenting the change in center of rotation with reverse total shoulder arthroplasty and its application to a consecutive series of 68 shoulders having reconstruction with one of two different reverse prostheses
Here are some recent relevant references.
Robert H. Cofield, MD, Award for Best Oral Presentation 2023: Up to 8 mm of glenoid-sided lateralization does not increase the risk of acromial or scapular spine stress fracture following reverse shoulder arthroplasty with a 135 degrees inlay humeral component Glenoid-sided lateralization in reverse shoulder arthroplasty (RSA) decreases bony impingement and improves rotational range of motion, but has been theorized to increase the risk of acromial or scapular spine fractures (ASFs). Up to 8 mm of glenoid-sided metallic lateralization did not appear to increase the risk of ASF when combined with a 135 degrees inlay humeral implant. Humeral distalization increased the risk of ASF, particularly when there is a larger change between pre- and postoperative AHD or higher inferior glenosphere overhang. In cases of pronounced preoperative superior humeral migration, it may be a consideration to avoid excessive postoperative distalization, but minimizing bony impingement via glenoid-sided lateralization appears to be safe.
Implant-Positioning and Patient Factors Associated with Acromial and Scapular Spine Fractures After Reverse Shoulder Arthroplasty Patient factors associated with poor bone density (inflammatory arthritis, osteoporosis, prior shoulder surgery, female sex, older age) and rotator cuff deficiency (massive rotator cuff tear, cuff tear arthropathy) appear to be the strongest predictors of ASFs and SSFs after RSA. To a lesser degree, final implant positioning may also affect ASF and SSF prevalence; increased humeral lateralization was found to be associated with lower fracture rates whereas excessive glenoid-sided and global lateralization were associated with higher fracture rates.
Predictive factors of acromial fractures following reverse total shoulder arthroplasty: a subgroup analysis of 860 shoulders This analysis showed that higher postoperative LSA, lower DSA and a lower ACHD (acromial/humeral distance) were predictive factors only for Levy type III fractures, but not for types I or II.
Incidence, risk factors, and complications of acromial stress fractures after reverse total shoulder arthroplasty Patient-specific factors that were independently associated with the occurrence of an ASF included osteoporosis, rheumatologic disease, shoulder corticosteroid injection within 3 months before surgery, and chronic oral corticosteroid use. Among patients with osteoporosis, the initiation of physical therapy within 6 weeks after surgery also increased the risk of ASF.
Acromial stress fractures and reactions after reverse total shoulder arthroplasty: a case-control study two factors were independently associated with the occurrence of an acromial stress fracture/reaction after RTSA: corticosteroids use and previous shoulder surgery.
Does prior rotator cuff surgery influence the outcomes and complications after reverse total shoulder arthroplasty in patients with cuff tear arthropathy or massive rotator cuff tear? A propensity score-matched study a history of prior rotator cuff surgery was associated with a high incidence of acromial stress fracture
Coracoacromial ligament integrity influences scapular spine strain after reverse shoulder arthroplasty This biomechanical study in cadavers examined the effect of coracoacromial (CA) ligament state (intact vs. released) and arm position on acromial and scapular spine strain following reverse total shoulder arthroplasty (rTSA). Scapular spine strain was quantified via 4 strain gauges placed along anatomic locations on the acromion and scapular spine. CA ligament release in the setting of rTSA resulted in increased scapular spine and acromial strain with the arm adducted, although these increases in strain were not statistically significant.
Low acromial insufficiency fracture rate in reverse shoulder arthroplasty with distal clavicle excision This study investigated the rate of acromial insufficiency fractures (AIF) in patients undergoing reverse shoulder arthroplasty (RSA) with concomitant distal clavicle excision (DCE). There were 3/174 acromial insufficiency fractures (1.7%). Twelve patients had insufficiency reactions (6.9%). Patients with acromial pathology were more likely to be female, and have a diagnosis of osteoporosis, and inflammatory arthritis. Unfortunately, there was no comparison group of RSAs without distal clavicle excision
Do preoperative scapular fractures affect long-term outcomes after reverse shoulder arthroplasty? Fractures identified on preoperative computed tomography scans were divided into 3 groups: (1) os acromiale, (2) multifragments (MFs), and (3) Levy types. Seventy-two shoulders had an occurrence of SSF. The multifragment fracture group has lower functional and satisfaction scores at all postoperative time points compared with both the nonfracture and the Os/Levy fracture group.
Acquired Acromion Compromise, Including Thinning and Fragmentation, Is Not Associated With Poor Outcomes After Reverse Shoulder Arthroplasty Preoperative acromial compromise was defined as follows: (1) thinning of the acromion (< 3 mm), which means a thickness of less than 30% of the normal acromion thickness (8 to 9 mm), and (2) acromial fragmentation. In patients with acquired acromial compromise-such as thinning or fragmented acromion because of advanced cuff tear arthropathy or previous acromioplasty, primary RSA resulted in no differences in functional outcome score, ROM, shoulder strength, and overall complications compared with patients without acromial compromise.
Variations in the Anatomic Morphology of the Scapular Spine and Implications on Fracture After Reverse Shoulder Arthroplasty This study evaluated the role of anatomic scapular morphology in acromion and scapular spine fracture (SSAF) risk after reverse shoulder arthroplasty (RSA). Scapular measurements were captured including scapular width measurements at the acromion (Z1), middle of the scapular spine (Z2), and medial to the first major angulation (Z3).
Patients with thicker acromions (Z1) and thinner medial scapular spines (Z3) had increased fracture risk. The mean zone 1 and 3 measurements for the control group were 18.6 ± 3.7 mm and 3.2 ± 1 mm, respectively, compared with 22.5 ± 5.9 mm and 2 ± 0.7 mm, respectively, in the SSAF cohort. This trend was also reflected in the calculated scapular spine proportion (SSP),Z1/Z3. A regression analysis was used to quantify the risk for scapular spine fracture after RSA as a function of SSP. Under this calculation, an SSP = 5 represented a <5% fracture risk; SSP = 9.2, 50%; SSP = 10.8, 75%; and SSP = 13.5, 95% risk.
Acromial and scapular fractures after reverse shoulder arthroplasty: comparison of 3018 reverse total shoulders by inlay and onlay humeral component design When comparing by inlay vs. onlay humeral component design, the rates of postoperative acromial or scapular spine fractures were statistically similar.
Reverse shoulder arthroplasty for patients with cuff tear arthropathy: do clinical outcomes differ by inlay vs. onlay design? At 2-year minimum follow-up, the position of the humeral tray in RSA prostheses (either inlay or onlay) for cuff tear arthropathy was not associated with PROs, shoulder ROM, or rates of complications, including baseplate loosening, acromial stress fracture, and scapular notching.
Increased Deltoid and Acromial Stress with Glenoid Lateralization and Onlay Humeral Stem Constructs in Reverse Shoulder Arthroplasty Finite element analysis was performed using a RSA system with both inlay and onlay configurations. Increased lateralization of the glenoid component resulted in increased levels of deltoid and acromial stress. For a given amount of glenoid lateralization, utilization of an inlay stem decreased acromial and deltoid stresses compared to onlay constructs.
High delta angle after reverse total shoulder arthroplasty increases stresses of the acromion: biomechanical study of different implant positions. High delta angle (combination of inferiorization and medialization of the center of rotation [COR]) after RTSA may be a risk factor for acromial fracture.
In a rigid body model of the upper extremity muscle, forces of the deltoid muscle were calculated before and after implanting RTSA in different arm and implant positions. High delta angles correlated with an increase in acromial stress. Both lateralization of the COR and the humerus decreased the acromial stress in this study. The lateralization of the humerus has the highest impact on acromial stress.These results are contrary to some in the current literature, thus further studies with focus on the acromial stress are needed.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link)
Shoulder rehabilitation exercises (see this link).