The critical shoulder angle (CSA) is the angle between a line connecting the superior and inferior aspects of the glenoid fossa (the glenoid inclination) and another line connecting the inferior aspect of the glenoid with the most inferolateral point on the acromion as seen on a plain anteroposterior radiograph.
A CSA >35 degrees has been associated with rotator cuff tears while a CSA <30 degrees has been is associated with primary glenohumeral arthritis. It has been suggested that a larger (more obtuse) CSA increases the elevating vector of the deltoid, leading to fatigue of the posterior-superior rotator cuff while smaller (more acute) CSA angles lead to increased compressive forces across the glenohumeral joint leading to wear of the glenoid joint surface.
A few issues come to the fore:
1. Does it seem reasonable that a change in the CSA by as little as 5 degrees would change the pathology of a shoulder from cuff disease to arthritis?
2. Is the CSA influenced primarily by glenoid inclination or by the position of the acromion?
3. What does CSA tell us about the acromion? The author of A prospective observational case control study investigating the coronal plane scapular morphological differences in full-thickness posterosuperior cuff tears and primary glenohumeral osteoarthritis, points out that the position of most inferolateral point on the acromion is affected both by the length and the height of the acromion: a longer acromion will increase the CSA
and a higher acromiom will decrease it.
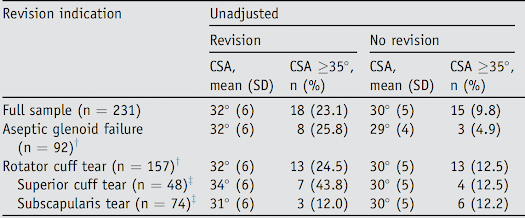
This article did not report glenoid inclination, so it is not known if the observed difference in CSA between revised and unrevised shoulderS is related to glenoid inclination or to acromial anatomy; it would be of interest to know whether shoulders revised for glenoid loosening and cuff failure had more superiorly inclined glenoids (see Anatomic total shoulder glenoid component inclination affects glenohumeral kinetics during abduction: a cadaveric study). Shoulders with increased CSA have been reported to have a higher prevalence of rotator cuff tears; the preoperative status of the rotator cuff is not presented for the patients in this series. The authors of The implications of the glenoid angles and rotator cuff status in patients with osteoarthritis undergoing shoulder arthroplasty found that in osteoarthritic patients, the CSA was higher in those with secondary osteoarthritis with torn rotator cuffs than in those with intact rotator cuffs and that the CSA was positively correlated with glenoid inclination.
5. Is there evidence that "correcting" a high CSA by lateral acromioplasty improves the outcome of rotator cuff surgery?
The authors of The Effects of Arthroscopic Lateral Acromioplasty on the Critical Shoulder Angle and the Anterolateral Deltoid Origin: An Anatomic Cadaveric Study found that in cadavers a 5-mm lateral acromion resection combined with an acromioplasty reduced the CSA from a mean of 34.3 degrees to a mean of 31.5 degrees. The authors of Arthroscopic Correction of the Critical Shoulder Angle Through Lateral Acromioplasty: A Safe Adjunct to Rotator Cuff Repair used lateral acromioplasty to reduce the mean CSA was reduced from 37.5° preoperatively to 33.9° postoperatively, but no clinical outcomes are presented. The authors of Lateral acromioplasty for correction of the critical shoulder angle used lateral acromioplasty to reduce the mean preoperative CSA from 39.7 ± 1.0°, to an average value of 32.1 ± 1.2° in patients having surgery for cuff disease, but clinical results are not presented. A review of the literature revealed one non-randomized retrospective case series that showed a small and inconsistent benefit of lateral acromioplasty Lateral Acromioplasty has a Positive Impact on Rotator Cuff Repair in Patients with a Critical Shoulder Angle Greater than 35 Degrees
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interestShoulder arthritis - what you need to know (see this link).How to x-ray the shoulder (see this link).The ream and run procedure (see this link).The total shoulder arthroplasty (see this link).The cuff tear arthropathy arthroplasty (see this link).The reverse total shoulder arthroplasty (see this link).The smooth and move procedure for irreparable rotator cuff tears (see this link).
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Shoulder rehabilitation exercises (see this link).