I. What is the definition of a failed shoulder joint replacement?
II. What are the types of shoulder joint replacement failure?
III. How is shoulder joint replacement failure evaluated?
IV. What can be done for shoulder joint replacement without revision surgery?
V. What are the surgical approaches to revision of a failed shoulder joint replacement?
Failure of anatomic shoulder joint replacement is discussed in this link.
Failure of reverse total shoulder joint replacement is discussed in this link.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link)
Popular Posts
- Do stemless total shoulders have lower revision rates because they are better than conventional total shoulders or because of confounders?
- Shoulder exercises
- Rotator cuff and rotator cuff tears - what you should know about them.
- X-rays for shoulder arthritis
- One of every eight primary total shoulder replacements required revision by 10 years - a causal analysis - augments/technology assistance
- Surgical failures: what causes them and how can we do better for our patients. Warning: this post is lengthly but informative!
- Shoulder arthritis - what you should know about it.
- What patients should know about shoulder joint replacement arthroplasty - FAQs
- Arthroplasty planning: CT-based and CT-free
- Of successful mammoth hunting and glenoid component failure - modeling causation
Sunday, June 4, 2023
When shoulder joint replacement for arthritis fails to give the desired result.
Friday, February 24, 2023
Managing the failed anatomic total shoulder

Polyethylene wear can cause osteolysis of the bone around the glenoid and humeral components leading to insufficient bone stock and bone quality for re-implantation.
Although there is a trend to manage failed anatomic total shoulder arthroplasties (aTSA) with revision to a reverse total shoulder arthroplasty, such revisions can be complicated by introperative fracture, difficulties in baseplate fixation, postoperative component loosening, instability, infection, neurologic injury and acromial or scapular spine stress fractures.
Some cases of failed aTSA can be successfuly revised to a hemiarthroplasty (HA).
The authors of Revision of total shoulder arthroplasty to hemiarthroplasty: results at mean 5-year follow-up investigated the outcomes reported by patients after conversion from aTSA to HA. Intraoperative glenoid or humeral component loosening was found in all 29 patients.
76% of the patients were satisfied with the procedure. Pain improved in 87% of the patients with mean pain scores improving significantly from 6.2 to 3.1. Simple Shoulder Test (SST) scores improved from a mean of 4.1 to 7.3. 62% had improvement exceeding the SST MCID threshold of 2.4. No significant differences in patient or shoulder characteristics were found in comparing those patients who improved by an amount greater than the MCID of the SST to those patients who improved less than the MCID. However, among the 6 patients who underwent conversion from aTSA to HA with cuff failure, only 3 (50%) attained MCID improvement of SST and 3 (50%) were satisfied with their revision.
59% of the patients had ≥2 positive cultures with the same bacteria; 82% of these were with Cutibacterium. Thus obtaining cultures at the time of revision is important. Furthermore, in view of the observation that over half of the revisions met the definition of having a periprosthetic infection (even though there were no obvious preoperative signs of infection), surgeons should consider complete, rather than partial, single-stage exchange and postoperative antibiotic therapy. Seven (88%) of the 8 patients with a loose humeral component had ≥2 positive cultures with the same bacteria. Surgeons should have an even higher index of suspicion for infection in cases of humeral component loosening.
Four patients (14%) required conversion to total shoulder arthroplasty: 2 to anatomic and 2 to reverse. An additional 3 patients (10%) had a revision HA performed because of persistent pain and stiffness.
There were no intraoperative fractures, problems with component fixation, infections, neurologic injuries or scapular stress fractures.
Comment: While the technique for revision of a failed total shoulder to hemiarthroplasty is not discussed in this paper, there are several options to be considered.
(1) Humeral head component removal, retention of a securely fixed humeral stem, glenoid component removal, debridement, culturing of deep tissue and explants for Cutibacterium, smoothing of the residual glenoid bone, insertion of a new humeral head with modifications of eccentricity, head diameter of curvature, and head thickness as needed to balance the shoulder's smoothness, mobility and stability, followed by a course of antibiotics until the results of the cultures are finalized. Some case examples of this method are shown below. In the case on the left, note the use of an inferiorly excentric humeral head component. In the case on the right, note the upsizing of the diameter of curvature to help distribute the load to the rim of the remaining glenoid bone. Glenoid bone grafting was not used in these cases.
(2) Complete single stage exchange with humeral head and body removal, glenoid component removal, debridement, culturing of deep tissue and explants for Cutibacterium, smoothing of the residual glenoid bone, insertion of a new body and a humeral head with eccentricity, head diameter of curvature, and head thickness as needed to balance the shoulder's smoothness, mobility and stability, followed by a course of antibiotics until the results of the cultures are finalized. The case for this approach is based on the observation that over 50% of cases in this study had culture evidence of periprosthetic infection (PJI), even in the absence of preoperative signs of infection. The problem is that the results of the cultures are not available in time to influence the surgical decision or the decision about antibiotics immediately after surgery. Complete single stage revision would seem to be particularly indicated in cases of humeral component loosening in view of the even higher association with PJI. (see Single-Stage Revision Is Effective for Failed Shoulder Arthroplasty with Positive Cultures for Propionibacterium). See the illustrative case below.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).
Sunday, November 6, 2022
Revising the failed anatomic total shoulder to a hemiarthroplasty
As an alternative, some cases of symptomatic glenoid loosining after aTSA can be effectively revised using a hemiarthroplasty (HA): removing the glenoid component and replacing the humeral head prosthesis to an implant that best fits within the remaining bony concavity (see examples below).

They studied twenty-nine patients who underwent a single stage conversion from aTSA to HA with mean follow-up of 4.5 years. 26 (90%) shoulders had glenoid component loosening, 8 (28%) had humeral component loosening, and 5 (17%) had both.
The subscapularis was found to be torn in 9 (30%), and the superior or posterosuperior cuff to be torn in 3 (10%).
Pain improved in 25 of 30 patients (87%); mean pain scores improved from 6.2 to 3.1.
Mean Simple Shoulder Test (SST) scores improved from 4.1 to 7.3;
18 of 29 patients (62%) had improvement above the SST MCID threshold of 2.4
22 of 29 (76%) of patients were satisfied with the procedure.
Revision surgery was required in 7 of 29 (24%) of patients. Two had reimplantation of anatomic polyethylene component, two had revision to reverse arthroplasty, and three patients had a revision hemiarthroplasty with complete single stage exchange for continued pain and stiffness.
Fifty-nine percent of patients (17 of 29) had ≥2 positive cultures with the same bacteria. Of these, 14 patients had ≥2 Cutibacterium cultures, 4 had ≥2 coagulase negative Staphylococcus (CoNS) cultures, and 1 had ≥2 cultures for both bacteria. Of the 8 patients that had humeral component loosening, 7 (88%) had 2 or more positive cultures with the same bacteria – 5 with Cutibacterium and 3 with CoNS.
.
Comment: As pointed out in a prior post, Managing the loose glenoid component after anatomic total shoulder arthroplasty, failed anatomic shoulder arthroplasty may be managed non operatively, by glenoid component removal and humeral head exchange, by reimplantation of an anatomic glenoid component, or by reverse total shoulder arthroplasty.
How might we consider these options?
The advantages of conversion of a failed anatomic total shoulder to a hemiathroplasty lie in
On the other hand, if glenoid failure is accompanied by failure of the rotator cuff, consideration should be given to reverse total shoulder as the first revision (among the 6 patients who underwent conversion from aTSA to HA with cuff failure, only 3 (50%) attained MCID improvement of SST and only 3 (50%) were satisfied with the results of their revision).
If glenoid failure is associated with humeral component loosening, this and prior studies report a very high rate (88%) of multiple positive deep cultures. In such a situation, harvesting multiple deep specimens for culture, humeral and glenoid component removal, thorough debridement, topical antibiotics and a course of postoperative antibiotics should be considered.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
To add this blog to your reading list in Google Chrome, click on the reading list icon

Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).
Thursday, October 13, 2022
Revision for failed anatomic total shoulder with a CTA hemiarthroplasty
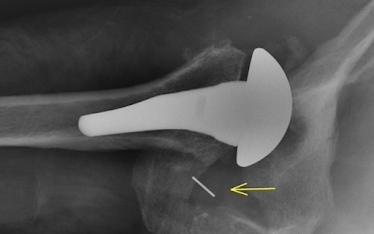
His postoperative films show centering of the humeral component in a concave glenoid.

Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interestShoulder arthritis - what you need to know (see this link).How to x-ray the shoulder (see this link).The ream and run procedure (see this link).The total shoulder arthroplasty (see this link).The cuff tear arthropathy arthroplasty (see this link).The reverse total shoulder arthroplasty (see this link).The smooth and move procedure for irreparable rotator cuff tears (see this link).Shoulder rehabilitation exercises (see this link).
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Tuesday, July 13, 2021
Failed total shoulder revised to ream and run
An active lady in her early 70's had a left total shoulder that became painful with use. She noted a "shifting" sensation when she elevated her arm.
At the time of presentation, her examination revealed a stiff painful shoulder with a slipping sensation on shoulder flexion.
Her x-rays showed a humeral component placed high in relation to the tuberosity
a loose glenoid component
placed on a retroverted glenoid
Wishing to avoid a reverse total shoulder, the patient desired to have a revision with complete prosthesis exchange to a ream and run procedure.
At surgery the loose glenoid component was easily removed, the well fixed humeral component was removed, cultures were obtained, the glenoid was reamed to a smooth concavity without attempt to change the version and without grafting the defect.
The immediate postoperative films are shown below.
The shoulder was started on immediate postoperative motion. Cultures were unremarkable at 3 weeks.
Seven years after her revision she presented because of arthritis in her right shoulder.
She states that her left shoulder is performing "normally". She demonstrated full active range of comfortable motion with no evidence of instability.
Her x-rays at 7 years after revision are shown below, demonstrating a regenerative soft tissue layer between the humeral head and the reamed glenoid.
Friday, September 11, 2020
Failed total shoulder - is arthroscopy useful?
These authors review the application of arthroscopy in evaluating unsatisfactory shoulder arthroplasties.
Perhaps the principal potential utility of arthroscopy is in the shoulder that is painful without obvious explanation. In this situation,
(1) multiple (ideally 5) tissue samples can be harvested for Cutibacterium cultures (14 days observation, aerobic and anaerobic media)
(2) the status of the glenoid can be assessed for wear or loosening
(3) capsular contractors and adhesions can be released
(4) the integrity of the rotator cuff and subscapularis can be assessed.
However, post arthroplasty arthroscopy can be technically difficult, especially if the shoulder is tight.
Our approach to total shoulder arthroplasty is shown in this link.
==
How you can support research in shoulder surgery Click on this link.
To see our new series of youtube videos on important shoulder surgeries and how they are done, click here.
Thursday, August 6, 2020
Reverse total shoulder in revision of failed anatomic arthroplasty - it's about glenoid bone stock.
The Effect of Glenoid Bone Loss and Rotator Cuff Status in Failed Anatomic Shoulder
Arthroplasty after Revision to Reverse Shoulder Arthroplasty
These authors evaluated outcomes and risk for re-revision in patients with a failed anatomic total shoulder arthroplasty (TSA) revised to reverse shoulder arthroplasty (RSA) based on rotator cuff deficiency and glenoid bone loss.
Fourteen patients were treated with retention of humeral stem and conversion to reverse shoulder arthroplasty using a convertible platform. Six of the revisions were performed as a staged procedure: two were due to infection, three were due to the severity of glenoid bone loss and one was due to intra-operative myocardial infarction. The five staged revisions for infection or glenoid bone loss had loose glenoids on preoperative radiographs.
Two year outcomes were available in 123 cases. The overall mean preoperative SST score was 2 with no significant difference in preoperative SST scores if the glenoid was fixed or loose (p=0.893) or if the rotator cuff was intact or deficient (p=0.627). The overall mean postoperative SST score was 5 with no significant difference in postoperative SST scores if the glenoid was fixed or loose (p=0.876) or if the rotator cuff was intact or deficient (p=0.234).
The overall re-revision rate was 11.4% with a mean time to re-revision of 22 months (range 0-89 months). The most common reason for subsequent revision was glenoid-sided failure (11/18). There were three RSAs revised for humeral loosening, three with subsequent infections, and one revised for instability. Of the 11 RSAs with glenoid sided failure, all had loose glenoids (100%) on preoperative radiographs at time of the initial revision. This is compared to 53.8% (n=85) cases with loose glenoids on preoperative radiographs in the group that were not subsequently revised (n=83) or those revised for reasons other than glenoid-sided failure (n=2, humeral loosening and infection, respectively). Rates of rotator cuff deficiency were similar between the revision groups.
The odds ratio was 1.8 for subsequent re-revision with glenoid loosening compared to those without loose glenoids on preoperative radiographs.
Comment: The success of anatomic and reverse total shoulder arthroplasties depends in large part on the preservation of glenoid bone stock. This is why the desire to change glenoid version needs to be curbed by the need to preserve bone. It is also why surgeons should carefully consider implants that would compromise glenoid bone stock should they need to be removed.
Saturday, February 15, 2020
Failed shoulder arthroplasties
These authors analyzed the epidemiology, etiologies, and revision options for 540 failed shoulder arthroplasties: 224 hemiarthroplasties (HAs), 237 anatomic total shoulder arthroplasties (TSAs) and 81 reverse total arthroplasties (RSAs) .
The indications for the initial arthroplasties differed by type of arthroplasty as shown below.
The indications for the first revision differed by type of arthroplasty as shown below.
Glenoid failure was a major indication for reoperation: erosion in HAs (29%) or loosening in TSAs (37%) and RSAs (24%). Instability was another major cause of reintervention: 32% in RSAs, 20% in TSAs, and 13% in HAs. Humeral implant loosening led to revision in 10% of RSAs, 6% of HAs, and 6% of TSAs.
An important finding of this study was the high rate of multiple revisions (21%) performed in the same patients, mainly attributable to unresolved soft-tissue insufficiency (26%) and/or infections (25%) as well as humeral bone loss; these may coexist with mechanical complications (glenoid or humeral loosening, instability).
The final implant was often an RSA, which has the potential to address combined bone and soft-tissue deficiencies.
Comment: The study of implant failure is vital to our understanding how we can do a better job of shoulder arthroplasty. The findings of this study need to be compared to those in three recent large studies, not included in the reference list:
Primary Shoulder Hemiarthroplasty: What Can Be Learned From 359 Cases That Were Surgically Revised?
What can be learned from an analysis of 215 glenoid component failures?
Analysis of 4063 complications of shoulder arthroplasty reported to the US Food and Drug Administration from 2012 to 2016
The authors of the third of these articles point out that most of the literature on shoulder arthroplasty failure comes from high-volume centers and that these reports tend to exclude the experience of community orthopedic surgeons, who perform most of the shoulder joint replacements.
They analyzed the failure reports mandated by the US Food and Drug Administration for all hospitals. Each reported event from 2012 to 2016 was characterized by implant, failure mode, and year of surgery.
The percentage distribution among the different failure modes was relatively consistent over the years of this study. Thus the question, "are we learning anything from these failures?"
For the 1673 anatomic arthroplasties, the most common failure modes were glenoid component failure (20.4%), rotator cuff/subscapularis tear (15.4%), pain/stiffness (12.9%), dislocation/instability (11.8%), infection (9%), and humeral component loosening (5.1%).
This study points to the utility of the freely accessible FDA MAUDE database as a resource for identifying failure modes for shoulder arthroplasty not readily identified in the published literature. Some modes of failure appear in the MAUDE data base long before they appear in the published literature, such as the dissociation of the glenosphere from the the baseplate as shown below.
We have a new set of shoulder youtubes about the shoulder, check them out at this link.
Wednesday, January 1, 2020
Failed total shoulder revised to a ream and run
Thursday, November 28, 2019
Failed short stemmed total shoulder revised to a ream and run
Her axillary "truth" view showed a posteriorly eccentric humeral head and posterior instability of the shoulder in a position of functional elevation of the arm.
The patient elected to have a single stage revision to a ream and run procedure. At surgery the glenoid component was loose. After the revision the patient was placed on the Red antibiotic protocol because of positive intraopertive cultures for Cutibacterium. At 6 months after her ream and run revision she had improved comfort and function with active elevation to 130 degrees. Her six month x-rays are shown below.
The axillary "truth" view showed the humeral head prosthesis centered in the glenoid.









































