Glenoid component loosening has been and remains an important cause of failure of anatomic total shoulder arthroplasty (data below from AOANJRR)
However, the survivorship of a pegged, cemented, cross linked, all-polyethylene glenoid component is excellent, with a 13 year cumulative percent revision rate of less than 5%. No metal backed or hybrid glenoid component has matched this outcome.


So, how might surgeons make the good results with the cemented, pegged all-polyethylene component even better? Here are some important concepts that can be put into action.
Careful preparation of the glenoid bone.
From the authors of Edge displacement and deformation of glenoid components in response to eccentric loading. The effect of preparation of the glenoid bone we learn that the wobble and warp of the polyethylene component is minimized by spherically reaming the bone to precisely match the back of the component.
Glenoid bone stock is preserved by reaming only enough to create a single concavity, rather than trying to "correct" glenoid version.
Assuring optimal seating and cementing of the component.
From the authors of The radiographic evaluation of keeled and pegged glenoid component insertion we learn that poor seating and poor cement technique contribute to poor fixation as evidenced by radiolucent lines on the immediate postoperative x-rays.
Poor seating is evidenced by the presence of cement between the glenoid bone and the backside of the component.
A thin layer of cement between the bone and component is brittle and subject to cracking, displacement and loss of support for the glenoid implant.
Optimal cementing is reflected by the absence of radiolucent lines on postoperative radiographs.
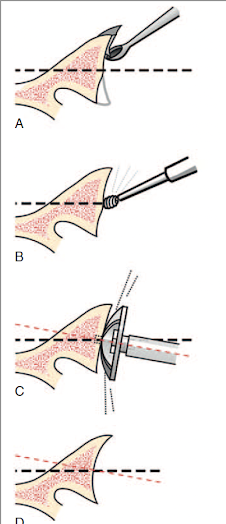
We have learned that this can be achieved by drying each fixation hole with a CO2 spray
Immediately before pressurizing the cement into the hole
Comment: The survivorship of cemented, pegged, all-polyethylene glenoid components has yet to be surpassed by other types of glenoid implants (see Total shoulder replacement stems in osteoarthritis-short, long, or reverse? An analysis of the impact of crosslinked polyethylene). Attention to the details of bone-preserving bone preparation, complete seating of the component and modern cement technique may further improve the clinical outcomes of anatomic total shoulder arthroplasty. Our technique for this procedure is shown in this link.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interestShoulder arthritis - what you need to know (see this link).How to x-ray the shoulder (see this link).The ream and run procedure (see this link).The total shoulder arthroplasty (see this link).The cuff tear arthropathy arthroplasty (see this link).The reverse total shoulder arthroplasty (see this link).The smooth and move procedure for irreparable rotator cuff tears (see this link).
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/