These authors analyzed the risk factors for, and compares the outcomes of patients with and without, acromial and scapular fractures in 4125 reverse total shoulders (rTSA) with a medialized glenoid/lateralized humeral implant.
Sixty-one of the 4,125 shoulders had radiographically identified acromial and scapular fractures.
After a minimum follow-up of 2 years, the rate of acromial and scapular fractures was 1.77%, with the fractures occurring at a mean (and standard deviation) of 17.7 ± 21.1 months after surgery. Ten patients had a Levy Type-1 fracture, 32 had a Type-2 fracture, 18 had a Type-3 fracture, and 1 fracture could not be classified.
Patients with acromial and scapular fractures were more likely to be female (84.0% versus 64.5%) to have rheumatoid arthritis (9.8% versus 3.3%), to have rotator cuff tear arthropathy (54.1% versus 37.8%), and to have more baseplate screws (4.1 versus 3.8 screws) than those without fractures.
Patients with fractures had significantly worse outcomes than patients without fractures, and the difference in mean improvement between these 2 cohorts exceeded the minimum clinically important difference for the majority of measures.
This multicenter study investigated the incidence of acromial stress fractures (ASFs) after reverse total shoulder arthroplasty (RTSA), and identified preoperative patient characteristics associated with their occurrence among 1479 patients undergoing either primary or revision RTSA between 2013-2018 with minimum 3-month follow-up.
ASFs were defined as radiographic evidence of an acromial or scapular spine fracture with clinical symptoms (e.g. tenderness over the acromion or scapular spine).
54 (3.7%) patients were diagnosed with an ASF after RTSA.
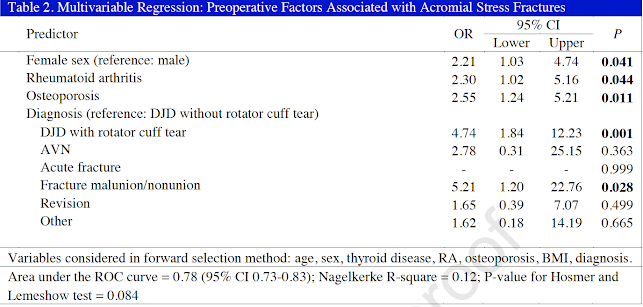
Patient-related factors independently associated with the development of an ASF included female sex (OR, 2.21)), rheumatoid arthritis (OR, 2.30), osteoporosis (OR, 2.55); , a diagnosis of degenerative joint disease (DJD) with rotator cuff tear (OR, 4.74), and fracture malunion/nonunion (OR, 5.21).
Comment: Acromial and scapular spine fractures are serious complications of RSA. While some of these fractures heal in good position, open reduction and internal fixation of displaced fractures is difficult and often unsuccessful.
In addition to the patient factors discussed in these two papers, other possible predisposing factors are being investigated, such as implant design and placement, screw number and placement, deltoid tension, as well as contact between the greater tuberosity and the acromion.
An important finding is that the average time for diagnosis of these fractures is over a year after the RSA.
Our practice is to perform as anatomic as possible RSA, avoiding unwanted contact and excessive tension while avoiding dangerous drill and screw placements and to advise patients regarding the risks of falls and of applying major loads to the reconstructed shoulder.
To see our technique for reverse total shoulder, click on this link.
To support our research to improve outcomes for patients with shoulder problems, click here.
How you can support research in shoulder surgery Click on this link.
To see our new series of youtube videos on important shoulder surgeries and how they are done, click here.