These authors point out that arthroscopic rotator cuff repair can be associated with substantial pain in the early postoperative period and that this pain can compromise the patient's quality of life and effective rehabilitation. A review of a cohort of over 18,000 patients that underwentoutpatient rotator cuff repair found that one of the most common complications resulting in readmission was pain, with 13% of readmissions occurring for this reason.
While opioids are used for analgesia following cuff repair, they are associated with potential dependence, abuse, and adverse side effects. While interscalene brachial plexus blocks may be helpful, they are limited by an effective duration of one to two days.
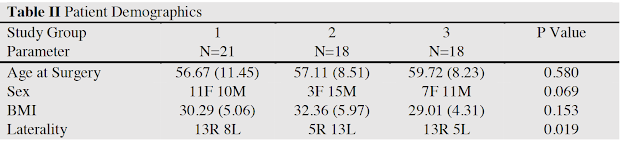
They conducted a randomized study of patients having arthroscopic cuff repairs comparing three groups:
57 patients (mean age, 57.8 ± 9.55 years) were included in this study.
Patients in group 3 took significantly fewer narcotics overall and took significantly fewer pills each day compared to group 2.
Group 3 also reported significantly better overall pain control compared to the other groups.
There were no significant differences in overall patient satisfaction between the groups.
There were no significant differences between groups regarding postoperative medication associated side effects.
Comment: It is interesting that rotator cuff repair is one of the more painful of shoulder procedures. Patients having RCR are in general much more uncomfortable and require more complex pain management that patients having joint replacement. For example, in this study all patients having cuff repairs received interscalene blocks with liposomal bupivacaine, whereas in our arthroplasty practice interscalene blocks are not needed (link).
These authors demonstrate the effectiveness of pre-emptive acetaminophen, i.e. acetaminophen given prior to surgery. This is shown to be an effective and safe means for lowering postoperative narcotic needs. They point out that acetaminophen has a plasma half life of 1.5-2.5 hours at lower doses, but the sulfonation pathway becomes saturated at higher doses (4g/day), allowing the half-life to increase. The patients in group 3 of this trial took the maximum recommended therapeutic dose (4 grams) the day before surgery. The lower threshold of a toxic dose is 12 grams, or 150-200mg/kg.