Using a query of the American Board of Orthopaedic Surgery (ABOS) Part II Oral Examination database for 2,633 cases of reverse total shoulders (RSA) performed by 9072 surgeons taking Part II boards from 2003 through 2017,
these authors sought to evaluate:
(1) the temporal trends in the incidence of and indications for RSAs performed by board-eligible orthopedic surgeons,
(2) the temporal trends in the incidence of reported complications after RSA, and
(3) the patient-related and surgeon-related variables that affected the reported complication rate.
They noted that the original 2004 FDA clearance for the reverse total shoulder was for massive RCT with DJD and an intact deltoid. They refer to other indications as being "off-label".
Over the period of this study, they found a 23 fold increase in the incidence of RSA (from 2.2 per 10,000 cases in 2005 to 50 per 10,000 cases in 2017) and a 19 fold increase in the proportion of candidates performing RSA.
They found an increasing trend seen in the proportion of primary and trauma cases and a declining trend in the proportion of revision cases.
They observed an increasing trend was seen in the proportion of RSA cases for "off-label" indications.
Shoulder fellowship-training was reported by 27% of the candidates, and these candidates performed less than half (42%) of all RSA procedures. The proportion of surgeons without shoulder fellowship training who performed RSA increased from 33% in 2005 to 80% in 2017. The number of RSA procedures per candidate among the fellowship-trained surgeons showed increasing trend from 1.5 in 2005 to 5.7 in 2017. This trend of number of RSA performed among non-fellowship trained candidates did not change over years.
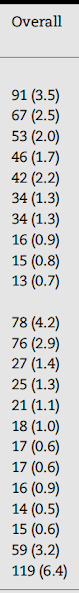
The complication rate over this time period was 34%; the incidence of medical, surgical and anesthesia complications was 18%, 15%, and 1.2%, respectively. Mortality, reoperation, and readmission rates were 0.6%, 3.2%, and 6.4%, respectively.
The incidence of complications increased over the study period from 32% in 2005 to 41% in 2017 - the majority of this increase was due to medical complications. The incidence of medical complications was associated with a diagnosis of proximal humeral fracture and with older patient age. The rate of mortality was increased for tumor related diagnoses. The incidence of surgical complications was increased for when RSA was performed for failed arthroplasty.
They did not find that shoulder fellowship-training experience was not associated with a decrease in any of the complications.
The 18% surgical complication rate for ABOS candidates performing RSA were 3 to 7 times greater than those reported in the literature and showed an increasing trend over the study period.
They concluded that there has been a dramatic increase in the use of RSA among board-eligible orthopedic surgeons in the United States since 2005, in part due to the increased use of the devices for indications other than rotator cuff deficiency+arthritis. The early complication rates for ABOS candidates performing RSA increased over a 10-year period. The complications were associated with older age, traumatic etiology, and revision surgery.
Comment: This is an interesting study that brings up some important questions.
(1) The complications reported by ABOS candidates are obviously captured in a manner that is different than complications reported in case series or population based registries. One might ask, are candidates for ABOS certification more or less likely to report complications than authors of case series or those entering data in to registries? In any event, conclusions about relative complication rates need to be interpreted in light of the different methods of data capture.
(2) The average followup for patients in this study was 10 weeks, much shorter than the typical two-year minimum for most published case series. In that many complications from RSA (loosening, dislocation, infection, periprosthetic fractures, acromial and spine fractures) occur at longer intervals after surgery. The high short term complication rate reported in this study is a concern.
(3) The indications for RSA have obviously expanded from the original "osteoarthritis with a deficient cuff", thus it is probably not appropriate to refer to the treatment of, for example, using RSA to treat a cuff deficient shoulder without arthritis but with pseudoparalysis as being "off label". On the other hand, it seems important to assess for what indications the FDA has cleared the use of RSA. For example, when is it appropriate to use an RSA rather than an anatomic TSA for an arthritic shoulder with an intact cuff?
(4) The increased rate of complications when RSA is used to treat proximal humeral fractures is expected in that the pathology is more complex and the patients are often less healthy than those with OA+cuff deficiency. Yet in current times, the use of RSA in managing complex fractures is generally accepted and would not be considered "off label". The same can be said for the use of RSA to manage failed primary arthroplasty
(5) As with any procedure, training and experience can be expected to increase competency. Other studies found a positive effect of fellowship training in increasing competency. . The number of cases to reach competency in performing RSA has been reported to range from 10-100. The suggested number of cases per year to maintain competency has been proposed to be 9. The relationship of case volume, experience and training in RSA needs further study.
(6) If indeed the patients of younger surgeons have a higher rate of complications with RSA and if fellowship training is not effective in reducing the rate of complications, serious consideration needs to be directed at methods for enabling these surgeons to perform this procedure more safely.
How you can support research in shoulder surgery Click on this link.