The goal of shoulder surgery outcome measurement is to capture the patient reported assessment of the condition of the shoulder before and after treatment for the highest percentage of patients having the procedure; in the words of E.A.Codman, "Every hospital should follow every patient it treats, long enough to determine whether or not the treatment has been successful, and then to inquire, 'if not, why not' with a view to preventing similar failure in future."
To achieve this goal, surgeons need a validated assessment tool that maximizes the ability of every patient to participate in long-term followup, minimizing the risk of non-reasponse bias (see this link). Potential barriers to achieving this goal include (1) restricting capture of followup data to those patients who are able to return to the providers office sequentially for long term followup and (2) restricting capture of followup data to those patients who are able effectively use a computer interface (see this link).
Shoulder arthroplasty outcomes are commonly assessed using validated measures such as the Simple Shoulder Test (SST) (see this link), the American Shoulder and Elbow Surgeons Score (ASES) (see this link), the Constant score (see this link) and the UCLA score (see this link). The first two of which (SST and ASES) are patient reported outcome measures (PROMs), emphasizing the ability to perform important activities of daily living; the SST and ASES assessments can be completed remotely without the patient needing to return to the provider's office, minimizing the risk of election bias, especially the risk of excluding those who are more remote and less able to afford repeated trips to visit the provider over the period of followup (a recent article, What is a Successful Outcome Following Reverse Total Shoulder Arthroplasty?, demonstrated that the easily accessible Simple Shoulder Test enabled 87% of the patients in the original sample to provide two year followup). The latter two (Constant and UCLA) require a provider to measure range of motion and/or strength thus a requirement for in person evaluation and incurring the potential for selection and observer bias.
The authors of Characteristics of Anatomic and Reverse Total Shoulder Arthroplasty Patients Who Achieve Ceiling Scores with 3 Common Patient Reported Outcome Measures have introduced another score, the Shoulder Arthroplasty Smart Score that requires a computer interface for scoring (see this link and this link). This score requires provider measurement of active forward elevation, internal rotation and external rotation in addition to three questions about pain and overall function. As shown in the slide below, there is low reliance on assessment of the patient's ability to perform activities of daily living (ADLs).
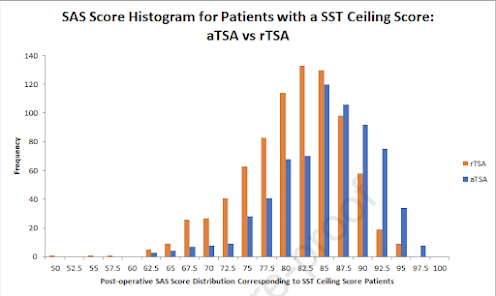
They used data from a database of a single shoulder prosthesis utilizing data from 30 different clinical sites to quantify and compare outcomes for 1817 anatomic (aTSA) and 2635 reverse (rTSA) patients using SST, ASES, UCLA, Constant, and SAS scores.
The number of aTSA and rTSA patients with ceiling scores were calculated and sorted into those that achieved ceiling scores and compared to patients without ceiling scores. A univariate and multivariate analysis then identified the patient demographics, comorbidities and implant and operative parameters associated with ceiling scores for each outcome measure.
They found that aTSA patients achieved ceiling scores at a significantly greater rate than rTSA patients for all outcome measures.
However to our knowledge it has not been demonstrated that a post arthroplasty shoulder with 180 degrees of active elevation and 90 degrees of external rotation would be more satisfactory or more functional than a shoulder with 140 degrees of active elevation and external rotation to 60 degrees (see Defining functional shoulder range of motion for activities of daily living, which concluded "Average shoulder motions required to perform the 10 functional tasks were flexion, 121° ± 6.7°; extension, 46° ± 5.3°; abduction, 128° ± 7.9°; cross-body adduction, 116° ± 9.1°; external rotation with the arm 90° abducted, 59° ± 10°; and internal rotation with the arm at the side, 102° ± 7.7°.")
With regard to the "ceiling effect" another recent article, Performance and responsiveness to change of PROMIS UE in patients undergoing total shoulder arthroplasty found that the ceiling effect for the SST in patients having aTSA was 18%.
In the graph below from The prognosis for improvement in comfort and function after the ream-and-run arthroplasty for glenohumeral arthritis: an analysis of 176 consecutive cases ...
..it can be seen a large number of patients having the ream and run for osteoarthritis "hit the ceiling" of 12 out of 12 on the SST. This means that
-the shoulder was comfortable at the side
-the shoulder allowed the patient to sleep comfortably
-the shoulder allowed reach to the small of the back to tuck in a shirt
-the shoulder allowed placement of the hand behind the head with the elbow straight out to the side
-the shoulder could lift a coin, a one pound weight, and an eight pound weight to the level of the top of the head without bending the elbow
-the shoulder allowed carrying 20 pounds at the side
-the shoulder allowed tossing a softball 20 yards underhand
-the shoulder allowed throwing a soft ball 20 yards overhand
-the shoulder allowed washing the back of the opposite shoulder
-the shoulder allowed work full time at the patient's usual job
In our view that's a pretty high ceiling; it is remarkable that so many patients can hit it after the ream and run. Obviously one could avoid the "ceiling effect" by adding a question such as, "would your shoulder allow you to throw 100 yards?", but it seems that "yes" responses to each of the 12 existing questions indicates a comfortable and highly functional shoulder.
In choosing an outcome measure for shoulder treatment, surgeons need to decide on their priorities.
In our practice we have found the SST to be broadly applicable to multiple procedures (arthroplasty, rotator cuff surgery, fracture surgery, etc), to be easily accessible to a broad range of patients without travel or socioeconomic barriers, valid (see this link), inexpensive, interpretable without a computer interface, and understandable to patients - rather than an abstract score, the SST reveals the outcome with respect to specific shoulder functions as shown below for aTSA for rheumatoid arthritis.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/