Complications and further surgery after reverse total shoulder arthroplasty
These authors prospectively collected clinical and radiological data of 797 patients who underwent
854 primary RTSAs performed by one of 11 fellowship-trained surgeons, using the Zimmer Biomet (USA) Anatomical Shoulder Inverse/Reverse RTSA.
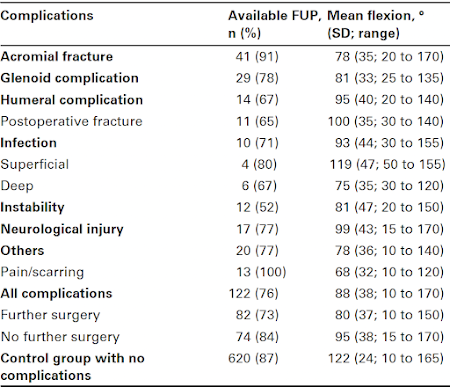
The overall surgical site complication rate was 22% (188 complications) in 152 patients (156 RTSAs; 18%) at a mean follow-up of 46 months (0 to 169).
The most common complications were
acromial fracture (in 44 patients, 45 RTSAs; 5.3%),
glenoid loosening (in 37 patients, 37 RTSAs; 4.3%),
instability (in 23 patients, 23 RTSAs; 2.7%),
humeral fracture or loosening of the humeral component (in 21 patients, 21 RTSAs; 2.5%), and
periprosthetic infection (in 14 patients, 14 RTSAs; 1.6%).
Other adverse events, such as haematomas, notching, heterotopic ossification, algodystrophy, radiolucent lines, and extravasation of cement, were not included in the complication rate.
The demographics and indications for the index rTSA for the patients with and without complications are shown in this table.
Further surgery was undertaken in 79 patients (82 RTSAs) requiring a total of 135 procedures (41% revision rate).
The most common indications for further surgery were
glenoid-related complications (in 23 patients, 23 RTSAs; 2.7%),
instability (in 15 patients, 15 RTSAs; 1.8%),
acromial fractures (in 11 patients, 11RTSAs; 1.3%),
pain and severe scarring (in 13 patients, 13 RTSAs; 1.5%), and
infection (in 8 patients, 8 RTSAs; 0.9%).
Kaplan-Meier curve below shows the survivorship to the first complication.The complication rate in this series of patients was 12% within the first year, 16% within the first two years, and 22% overall.
Patients who had a complication had significantly worse mean Constant scores (57% (SD 24%) vs 81% (SD 16%)) and Subjective Shoulder Value (SSV) scores (53% (SD 27%) vs 80% (SD 20%)) compared with those without a complication.
The impact of these complications on shoulder function (in comparison to uncomplicated rTSAs) was substantial, worst for acromial fracture, pain/scarring and deep infection.
If revision surgery was necessary, the outcome was even further compromised (mean rCS score: 51% (SD 23%) vs 63% (SD 23%); SSV score: 4% (SD 25%) vs 61% (SD 27%).
The high rate of complications is notable in view of the facts that (1) the surgeries were performed by fellowship trained surgeons, (2) this series did not include revisions of prior arthroplasties and only a few fractures - two diagnoses that are associated with high complication rates, and (3) the cumulative complication rate continued to increase with time (suggesting that longer term followup would reveal an even higher rate of complications).
The rate of complications and further surgery in this study is similar to that reported in Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review of 782 cases (24% and 13%).
Use of the reverse total shoulder (rTSA) is growing rapidly, now including its application to diagnoses that are traditionally well managed with less complication-prone surgeries, such as osteoarthritis in shoulders with an intact rotor cuff (which can be effectively managed with an anatomic total shoulder) and cuff tear arthropathy with retained active elevation (which can be effectively managed with a cuff tear arthropathy arthroplasty).
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/