Its insertion requires concentric reaming of the anterior glenoid
or a superior/inferior scraper
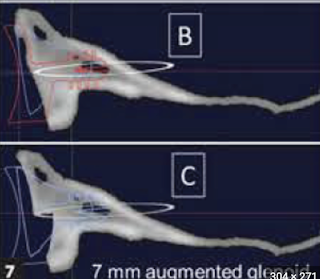
The size of posterior augment ranges from 3 to 7 mm. The amount of bone removed in a case using a 7 mm augment is shown below.
50 patients (57%)(41 B2 and 9 B3 glenoids) with minimum 2 year followup were included in the analysis. Two patients having posterior dislocation were excluded.
There was strong agreement among the observers for preoperative and postoperative glenoid version as measured on plain x-rays.
Range of motion was improved over preoperative values.
Preoperative glenoid retroversion did not significantly affect the postoperative range of motion.
Postoperative glenoid component retroversion and residual posterior subluxation relative to the scapular body or glenoid face did not correlate with range of motion in any plane.
Preoperative shoulder SANE and VAS scores were missing from this study. The mean postoperative VAS score was 0.5 and mean SANE score was 94.5
Posterior subluxation relative to the glenoid face was moderately associated with lower SANE scores.
While the amount of posterior decentering of the humeral head was reduced from a mean of 21 percent before surgery to 3 percent after surgery, the amount of glenoid version was only changed by 7 degrees (24 degrees to 17 degrees).
Comment: The questions needing answers are
(1) how important is version correction to a value of 15 degrees or less as proposed by some authors?
(2) while it is evident that postoperative posterior decentering can lead to eccentric loading and rocking horse loosening of the glenoid component
is "correction" of glenoid version necessary for re-centering the humeral head on the glenoid?
(3) are the results of anatomic shoulder arthroplasty with a standard glenoid component for B2 and B3 glenoids inferior to those for glenoid types A1 or A2?
(4) are the clinical results of anatomic shoulder arthroplasty for B2 and B3 glenoids using an augmented component superior to those obtained with a standard glenoid component?
Some of the answers may be found in Anatomic Total Shoulder Arthroplasty with All-Polyethylene Glenoid Component for Primary Osteoarthritis with Glenoid Deficiencies.These authors sought to evaluate the ability of shoulder arthroplasty using a standard glenoid component to improve patient self-assessed comfort and function and to correct preoperative humeral-head decentering on the face of the glenoid in patients with primary glenohumeral arthritis and type-B2 or B3 glenoids. They identified 66 shoulders with type-B2 glenoids (n = 40) or type-B3 glenoids (n = 26) undergoing total shoulder arthroplasties with a non-augmented glenoid component inserted without attempting to normalize glenoid version and with clinical and radiographic follow-up at a minimum of 2 years. Shoulder pathoanatomy was characterized on the axillary "truth" view in terms of glenoid version (angle between lines G and S) and humeral head decentering on the face of the glenoid (distance between line P - the perpendicular bisector of line segment G - and the center of the humeral head, C). Preoperative CT scans and computer planning software were not used in this case series.
This method allowed direct comparison of glenoid version and humeral decentering before and after the arthroplasty
The Simple Shoulder Test (SST) score improved from 3.2 points preoperatively to 9.9 points postoperatively at a mean time of 2.8 years for type-B2 glenoids and from 3.0 points preoperatively to 9.4 points postoperatively at a mean time of 2.9 years for type-B3 glenoids. These patient reported outcomes were as good as those achieved with other glenoid types.
These outcomes were achieved without changing glenoid version: postoperative glenoid version was not significantly different from preoperative glenoid version.The rates of bone integration into the central peg for type-B2 glenoids (83%) and type-B3 glenoids (81%) were not inferior to those for other glenoid types (A1 67%, A2 85%, B1 74%, D 75%).
Anterior penetration of the glenoid neck by the central peg of the glenoid component was observed in 2 (11%) of 19 of the type-B1 glenoids, in 6 (15%) of 40 of the type-B2 glenoids, and in 6 (23%) of 26 of the type-B3 glenoids. Perforation of the glenoid by the central peg was not associated with inferior clinical or radiographic outcomes. Twelve of the 14 shoulders with glenoid neck penetration had ingrowth of bone between the flanges of the central peg with no radiographic evidence of component loosening. The final mean SST score for the 14 shoulders with central peg penetration was 9.4 points, a value not significantly different from that for all of the type-B2 and B3 glenoids (9.7 points).
This study demonstrates that good two year clinical outcomes can be achieved for B2 and B3 glenoid components using a standard (non-augmented) glenoid component inserted without changing glenoid version.
Further clinical research will be required to establish clinical practice guidelines and appropriate use criteria for augmented glenoid components.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).