While some surgeons routinely perform acromioplasty in conjunction with cuff repair, there is only minimal evidence to support a clinically significant benefit in terms of patient reported outcomes:
Acromioplasty combined with arthroscopic rotator cuff repair can reduce the risk of reoperation: a systematic review and meta-analysis. "Combining arthroscopic cuff repair with acromioplasty can reduce the rate of reoperation, especially in patients with type 3 acromion, but it provides no clinically important change in the retear rate and postoperative patient reported outcomes compared with arthroscopic cuff repair without acromioplasty"
Chochrane on rotator cuff repair "Not surprisingly, there were no observed benefits to acromioplasty in terms of pain, function, or health-related quality of life—a finding that has been known for some time and is based on several high-quality randomized controlled trials"
Efficacy of concomitant acromioplasty in the treatment of rotator cuff tears: A systematic review and meta-analysis "our present study demonstrated that acromioplasty treatment is significantly superior to nonacromioplasty in shoulder pain relief at 12 months postoperatively and in ASES score improvement at the final follow-up in conjunction with rotator cuff repair. However, these statistically significant differences were not clinically relevant. Thus, there were no differences in shoulder function or pain scores for patients undergoing rotator cuff repair with and without acromioplasty."
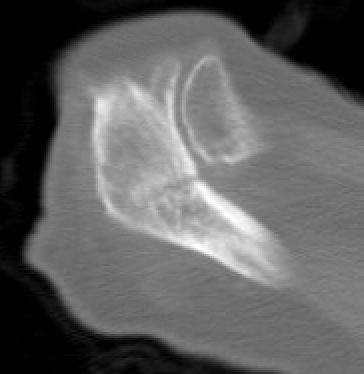
In addition, there is evidence that sacrifice of the coracoacromial arch can increase the risk of acromial stress fractures.
The authors of Prior Subacromial Decompression is a Significant Risk Factor for Development of Acromial Stress Fracture After Reverse Total Shoulder Arthroplasty sought to determine if prior acromioplasty increases the risk of these fractures after reverse total shoulder arthroplasty (rTSA). 106,599 patients undergoing primary rTSA were identified. One out of 100 patients sustained an acromial stress fracture. Prior acromioplasty was a significant independent risk factor, conferring a 26% higher risk. Additional independent risk factors for these fractures included increased Charlson Comorbidity Index, history of a rotator cuff tear, osteoporosis and inflammatory arthropathy.
In performing rotator cuff repair, surgeons need to balance the possible advantages of acromioplasty against the increased risk of acromial / spine fractures should subsequent reverse total shoulder arthroplasty become necessary.
Obesity and total joint arthroplasty: Does weight loss in the preoperative period improve perioperative outcomes? assessed whether a 10% weight loss prior to TJA had a impact on perioperative and 30-day outcomes in obese patients. The authors found no difference between groups with or without weight loss in terms of operative time, length of stay, discharge destination, or 30-day adverse events, including complications, re-admissions, re-operations, and mortality.
Malnourished patients had significantly higher risks of 90-day major complications, including sepsis, myocardial infarction, readmission, pneumonia, renal failure, and blood transfusion. These patients were also at increased risk of periprosthetic infection and surgical revision within 2 years after arthroplasty.
Consultation with an experienced nutritionist and social support are indicated for malnourished patients. The patients need to be advised that the necessary dietary changes can be difficult and may take months or longer to create a meaningful reduction in surgical risk.
While it is commonly recognized that cigarette smoking increases the risk of surgical complications, patients may wish to continue their use of other forms of tobacco. The authors of Effects of Smokeless Tobacco Use on Primary Total Shoulder Arthroplasty Outcomes compared outcomes between smokeless tobacco users and nontobacco users. They found that patients using smokeless tobacco had higher average Charlson-Deyo Comorbidity Indices and concomitant alcohol use and lower socioeconomic status. Smokeless tobacco users had higher rates of acute respiratory disease syndrome, sepsis, and mortality at 180 days. These adverse outcomes are attributed to the vasoconstriction, impaired tissue oxygenation, and immunosuppression occurring with tobacco use. Tobacco use predicts a more difficult episode of care after anatomic total shoulder arthroplasty pointed out that current tobacco use is associated with increased postoperative pain.
As every orthopaedic surgeon knows, osteoporosis predisposes patients to fractures and failure of joint reconstructions. One in four women over the age of 65 has this condition. Because there is a high prevalence of undiagnosed or untreated osteoporosis, surgeons need to screen patients with risk factors for this common condition: female, advanced age, low BMI, malnourishment, inflammatory arthropathy, steroid medication, inactivity, and poor diet. The authors of Anti-osteoporotic treatment reduces risk of revision following total shoulder arthroplasty in patients with osteoporosis investigated whether anti-osteoporotic therapy correlates with improved revision outcomes following total shoulder arthroplasty.
Patients with a preoperative diagnosis of osteoporosis were stratified into 2 groups: (1) patients with osteoporosis who underwent anti-osteoporotic therapy within 6 months prior to surgery (anti-OP cohort) and (2) patients with osteoporosis who never received anti-osteoporotic treatment (no anti-OP cohort).
In total 40,532 osteoporotic patients were included, with 11,577 (28.5%) having undergone anti-osteoporotic treatment.
Patients who did not receive anti-osteoporotic treatment had significantly higher odds of 2-year all-cause revision and mechanical loosening following TSA when compared to those treated for osteoporosis.
Simple steps can reduce the risk of osteoporosis: a diet with substantial protein (e.g. at least 1/2 gram of protein/pound of body weight), fat and calories, Vitamin C and D supplementation, calcium supplementation, and general bone-loading exercise (e.g. walking, rowing machine). Be aware of the "tea and toast" diet and inactivity. Patients at risk should be monitored with DEXA scans. Formal anti-osteoporotic treatment should be administered by a physician knowledgeable about metabolic bone disease.
Managing Anemia
Anemia (e.g preoperative hemoglobin < 13.5 g/L) is present in up to one of three patients having shoulder arthplasty.
Complications Associated with Preoperative Anemia and Risk Factors for Blood Transfusion after Shoulder Arthroplasty: A Systematic Review found the patients with preoperative anemia (PA) demonstrated a 24.4% complication rate in comparison to 8.8% in those without such a diagnosis. Stratification by PA severity revealed a 34.9% complication rate in patients with moderate to severe PA. In patients with PA, pulmonary complications were the most prevalent followed by thromboembolic, renal, and postoperative transfusion-related complications.
Lower preoperative hemoglobin and revision shoulder arthroplasty were correlated with a higher risk of postoperative transfusion.
Because anemia is associated with chronic illness and malnutrition, it is difficult to know how much of the adverse effect is due to the anemia itself or to the underlying condition that may be contributing to it. Thus the management of PA is complicated.
Erythropoiesis-stimulating agents can increase hemoglobin levels but carry potential risks (e.g., thromboembolic events), particularly in older populations.There is no strong evidence that administration of erythropoietin (EPO) significantly reduces complication rates in anemic patients undergoing shoulder arthroplasty.
There is currently no strong evidence that preoperative blood transfusion lowers complication rates in mild or moderately anemic patients undergoing shoulder arthroplasty. In fact, preoperative transfusion may increase the risk of complications in some cases. Allogeneic blood transfusion, including preoperative transfusion, is associated with increased risk of surgical site infection, increased thromboembolic events and immunomodulatory effects.
In patients with ferritin <30 ng/mL or transferrin saturation <20%, oral or especially intravenous iron may be the most cost effective approach for raising serum hemoglobin before surgery
Notably, tranexamic acid (TXA) is effective in reducing blood loss and transfusion need; this medication is now in common use in patients having shoulder arthroplasty and has been found to have a very low rate of adverse reactions
Inspiring the patient
Finally, as surgeons we have an opportunity to inspire the patient to take responsibility for their own health as detailed here.
Conclusion
In order to do our very best for each of our patients, we need to be on the watch for and to manage the factors that may threaten the outcome of their shoulder arthroplasty.
At a young age, barred owls learn to be watchful for threats
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link)
Shoulder rehabilitation exercises (see this link).