The published evidence indicates that postoperative prosthetic glenoid retroversion is not associated with worse patient outcomes after anatomic total shoulder arthroplasty.
Rather than the amount of retroversion, the quality of the seating of the glenoid component appears to be the primary driver of the clinical outcome.
Let's look at some recent articles from the peer-reviewed literature
The authors of Anatomic Total Shoulder Arthroplasty with All-Polyethylene Glenoid Component for Primary Osteoarthritis with Glenoid Deficiencies used standard all polyethylene non-augmented glenoid components inserted without attempt to "correct" glenoid retroversion in managing glenohumeral arthritis in patients with types A1, A2, B1, B2, and B3 glenoid pathoanatomy.
The authors of Does glenoid version and its correction affect outcomes in anatomic shoulder arthroplasty? A systematic review evaluated studies on the effect of preoperative and postoperative glenoid retroversion on clinical functional and radiologic outcomes in patients who underwent anatomic TSA. They concluded that there is currently insufficient evidence that pre- or postoperative glenoid version influences postoperative outcomes independent of other morphologic factors such as joint line medialization. Given that noncorrective reaming demonstrated favorable postoperative outcomes, and postoperative glenoid version was not significantly and consistently found to impact outcomes, these authors find that there is inconclusive evidence that correcting glenoid retroversion is routinely required.
The authors of Factors associated with functional improvement after posteriorly augmented total shoulder arthroplasty pointed out that posteriorly augmented glenoid components in anatomic total shoulder arthroplasty attempt to address posterior glenoid bone loss but have inconsistent clinical results. They performed a retrospective review of 50 patients who underwent TSA with a step-type augmentation performed by a single surgeon between 2009 and 2018. Glenoid morphology included type B2 glenoids in 41 patients and type B3 glenoids in 9. Postoperative ROM and function showed no clinically important associations with postoperative glenoid retroversion. Component loosening was frequent among shoulders with 7 mm augmentation.
The authors of Do glenoid retroversion and humeral subluxation affect outcomes following total shoulder arthroplasty? investigated in 113 patients whether glenoid retroversion and humeral head subluxation were associated with inferior outcomes after TSA and whether change of retroversion influences outcomes after TSA. They found no correlation between postoperative glenoid version or humeral head subluxation and ASES scores. For patients with preoperative retroversion of >15 degrees , there was no difference in outcome scores based on postoperative retroversion. There were no differences in preoperative or postoperative version for patients with or without glenoid lucencies. They observed no significant relationship between postoperative glenoid retroversion or humeral head subluxation and clinical outcomes in patients following TSA.
The authors of Glenoid component retroversion is associated with osteolysis found that postoperative glenoid component retroversion was correlated with osteolysis around the glenoid center peg but that the presence of osteolysis around the center peg was not correlated with a worse clinical outcome defined by shoulder scores or a reoperation due to glenoid loosening.
The authors of Total shoulder arthroplasty in patients with a B2 glenoid addressed with corrective reaming: mean 8-year follow-up reviewed 59 patients finding that glenoid component failure was associated with worse initial glenoid component seating but that there was no association between glenoid component failure and preoperative retroversion, inclination, or humeral head subluxation.
The authors of Total shoulder arthroplasty outcomes after noncorrective, concentric reaming of B2 glenoids reviewed their outcomes for 51 patients with B2 glenoids having a mean retroversion of 19.1 degrees (range 5.4 degrees -38 degrees ) who were treated with non-corrective reaming. These patients had significant improvement in clinical outcome scores, high patient satisfaction, and high survivorship ( implant survivorship rate was 95% at a mean follow-up of 4.9 years).
Glenoid retroversion does not impact clinical outcomes or implant survivorship after total shoulder arthroplasty with minimal, noncorrective reaming in 151 anatomic total shoulder arthroplasties the mean preoperative retroversion was 15.6 degrees. Total shoulder arthroplasty was performed without corrective reaming. Higher values of retroversion were not associated with early deterioration of clinical outcomes, revisions, or failures.
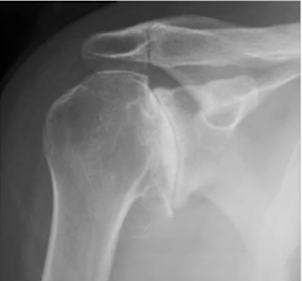
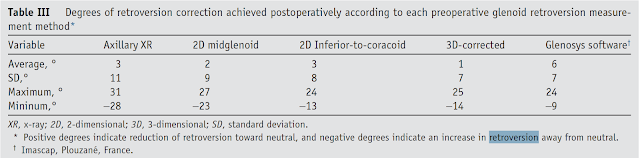
As we see from the above measurements of glenoid version are important to understanding and managing glenohumeral pathoanatomy. A recent article reviewed glenoid version measurements before and after shoulder arthroplasty:Inconsistencies in Measuring Glenoid Version in Shoulder Arthroplasty: A Systematic Review. They considered 61 studies encompassing 17,070 shoulder arthroplasties. Less than half (44%) of these described explicitly how glenoid version was measured. Often different methods were used to measure version before and after arthroplasty: preoperartive glenoid version was assessed using computed tomography in 75% of the cases; by contrast, over 50% of the studies that measured postoperative version used axillary radiographs. If we are to understand the preoperative to postoperative changes in glenoid version, we need for the measurements to be made using the same imaging modality.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).