Many different shoulder outcome measures have been proposed.
Some ask the patient: "How would you rate your shoulder function as a percentage of normal, with 0% being completely nonfunctional and 100% being completely normal?" or "How would you rate your shoulder today as a percentage of normal, where 0% represents no function and 100% represents normal function?".
Some ask the patient to make a mark on a visual analogue scale
Some ask for a measurement of range of motion that is included in an overall score
Some use computer adaptive testing to derive a single number representing pain and function.And still others generate a single number based on "hands-on" evaluation of strength and motion by a trained observer combined with patient answers to questions about pain and function.
While each of these may have advantages, my preferred outcome measure is simple, easily accessible to almost all patients, and reflects what the patient believes they can do with their shoulder.
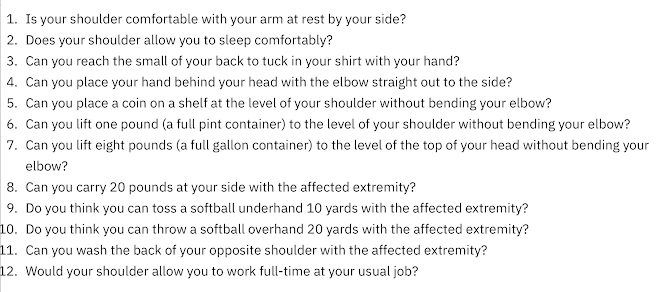
It is the Simple Shoulder Test, a set of twelve "yes" or "no" shoulder function questions:
- Is your shoulder comfortable with your arm at rest by your side?
- Does your shoulder allow you to sleep comfortably?
- Can you reach the small of your back to tuck in your shirt with your hand?
- Can you place your hand behind your head with the elbow straight out to the side?
- Can you place a coin on a shelf at the level of your shoulder without bending your elbow?
- Can you lift one pound (a full pint container) to the level of your shoulder without bending your elbow?
- Can you lift eight pounds (a full gallon container) to the level of your shoulder without bending your elbow?
- Can you carry 20 pounds at your side with the affected extremity?
- Do you think you can toss a softball underhand 10 yards with the affected extremity?
- Do you think you can throw a softball overhand 20 yards with the affected extremity?
- Can you perform your usual work?
- Can you perform your usual sport?
Completion of the SST requires only a pencil and a stamped envelope.
As a result use of the SST avoids the risk of selection bias that can result from excluding those who cannot use a computer or who cannot travel for in a person examination. It also avoid the problems of observer bias and inter-observer variability; the consistent observe this the most important one: the patient.
The easy accessibility of the SST enables long term studies with low percentages of "lost to followup".
Since its introduction by Doug Harman and Steve Lippitt in 1993 it has been used in 1,637 publications in peer reviewed journals at the time of this post and has been translated to and validated in multiple languages, including Spanish, French, German, Italian, Chinese, Japanese, Korean, Portuguese, Dutch, Swedish, Turkish, Russian, Arabic, Hindi, Thai, and Bulgarian, enabling cross-cultural studies.
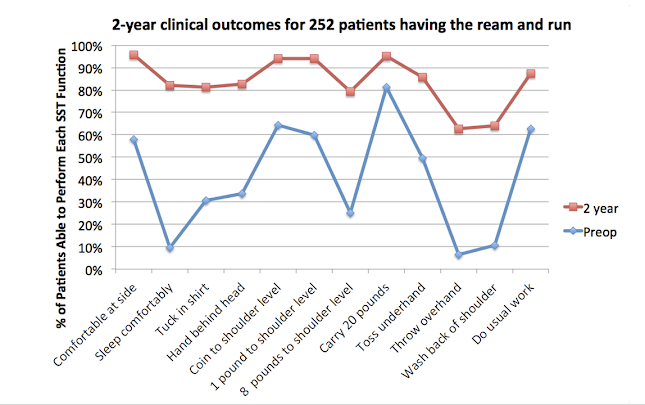
Instead of yielding a single numerical score (which may have limited meaning to our patients), the SST gathers easily understandable information about the individual's ability to perform 12 separate function. This enables surgeons and patients to understand the ability of a procedure to address the functional deficits of particular importance to the individual.
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link)
Shoulder rehabilitation exercises (see this link).