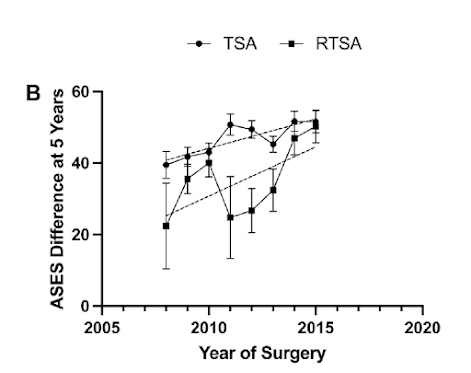
There are a host of variables that may affect the clinical outcome of reverse total shoulder arthroplasty. A number of authors have attempted to relate distalization and lateralization to outcome scores. For example in Managing rotator cuff tear arthropathy: a role for cuff tear arthropathy hemiarthroplasty as well as reverse total shoulder arthroplasty, the authors found that the postoperative position of the center of rotation and greater tuberosity on anteroposterior radiographs did not correlate with the clinical outcomes for either procedure.
The authors of How To Choose The Best Lateralization And Distalization Of The Reverse Shoulder Arthroplasty To Optimize The Clinical Outcome In Cuff Tear Arthropathy investigated the effect on the 1 year ASES score of combinations of lateralization and distalization of 62 patients having reverse total shoulder arthroplasty performed for cuff tear arthropathy. They measured lateralization by the LSA as shown below

and distalization by the DSA as shown below.

They found the correlation between ASES score and LSA to be = -0.43 and the correlation between ASES score and DSA to be 0.39; both values lying in the "moderate" range.
The accepted value for minimal clinically important difference for the ASES score in total shoulder arthroplasty is 20.9
The DSA of patients with ASES scores > 76 was 48.55 while the DSA of patients with ASES scores < 76. was 37.82, a difference of 10.7.
The LSA of patients with ASES > 76 was 86.43 while the LSA of patients with ASES scores <76 was 100.09, a difference of 13.7.
Thus neither measurement exceeded the threshold for clinical significance.
The authors suggest that optimal LSA should be no more than 90.5° yet of the 24 patients with LSA > 90.5 degrees 75% had ASES scores >76. Furthermore, what should be the lower limit of the LSA?

The authors also suggest that the optimal DSA should be no less than 37.5°, yet of the 17 with DSA less than 37.5, 65% had ASES scores >76. Furthermore, what should be the upper limit of the DSA?

Comment: This is a well done study that effectively uses scatter plots to show all their data. This type of presentation lends itself to an understanding of the variability in the studied relationships.
As the authors point out in their discussion, prior authors have come to varying conclusion about the clinical (rather than statistical) significance of the relationships between distalization angles and lateralization angles.
It seems curious that distalization (a linear dimension) is being measured as an angle, rather than as a linear dimension (see yellow line) and

that laterialization (a linear dimension) is being measured as an angle, rather than as a linear dimension (see yellow line).

Both lateralization and distalization affect deltoid tension, moment arms, center of rotation, stretch on the brachial plexus, the stabilizing compressive force across the articulation, the function of the remaining cuff muscles, the ability to repair the subscapularis and more. We need to know what is the "sweet spot" when the effects of these two variables are considered together?
Follow on twitter/X: https://x.com/RickMatsen
Follow on facebook: https://www.facebook.com/shoulder.arthritis
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).