Glenohumeral instability is one of the most common disabling conditions of the shoulder. Yet given the great flexibility of the joint and the small, shallow socket provided by the glenoid
it is a wonder that the shoulder remains as stable as it does with everything we ask it to do
In order to understand, evaluate and manage shoulder instability, one needs to understand how the joint is normally stabilized. Our late fellow, Doug Harryman, did a great job explaining shoulder stability in these two videos: Shoulder Mechanics 1 and Shoulder Mechanics 2.
The principles of shoulder stability are detailed in Chapter 3 of the freely available Practical Evaluation and Management of the Shoulder (see this link.).
While the knee is stabilized by ligaments that remain isometric through its range of flexion and extension, the shoulder has no isometric structures that limit its range of motion. The surrounding soft tissues remain lax in most functional positions of the shoulder, except those performed at the extremes of shoulder motion (such as in the baseball pitch shown above).
While the hip is stabilized by a deep acetabular socket (which limits hip range of motion when its rim is contacted by the femur), the shoulder's socket is shallow, allowing it a great range of impingement-free motion.
The essential mechanism stabilizing the shoulder is concavity compression, a mechanism that functions throughout the range of shoulder motion. Just as the compressive effect of gravity stabilizes the golf ball in the small, shallow concavity of the tee
the glenohumeral joint is stabilized when the net force on the humeral head compresses it into the small, shallow glenoid concavity of the glenoid
As long as the net force acting on the humeral head passes within the glenoid concavity, the joint is stable. The glenoid arc provides a range of positions in which this condition can be met.
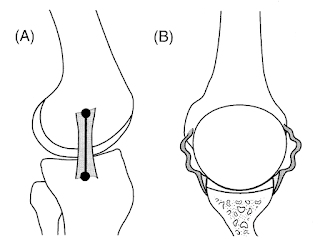
The glenoid bone, cartilage and labrum each contribute to the concavity.
The concavity is less in the anteroposterior direction than in the superiorinferior direction.
As a result, the joint's stability from front to back is less than its stability from top to bottom.
If the concavity is compromised, the range of stable positions is reduced.
Stability is also compromised if the net force is not directed within the glenoid concavity.
Fortunately, the scapula can usually be positioned so that the concavity is aligned with the compressive force.
For example, if the hand pushes forward while the scapula is retracted, the force on the humerus is not aligned with the glenoid socket and stability is threatened.
However, if the hand pushes forward while the scapula is protracted, the force on the humerus is closely aligned with the glenoid socket, so stability is optimized.
The specifics of surgical treatment for glenohumeral instability are beyond the scope of this post. However, understanding the concavity compression mechanism of shoulder stability can help guide practice:
(1) when instability results from deficiencies in the labrum, cartilaginous lip, or glenoid bone, consider restoring the glenoid concavity through Bankart repair or bony procedures
(2) when instability results from malalignment of the net humeral force with the glenoid, consider restoring the constraints to excessive motion, using capsular repair/shift, rotator interval plication and/or remplissage.
You can support cutting edge shoulder research that is leading to better care for patients with shoulder problems, click on this link.
Follow on twitter: https://twitter.com/shoulderarth
Follow on facebook: click on this link
Follow on facebook: https://www.facebook.com/frederick.matsen
Follow on LinkedIn: https://www.linkedin.com/in/rick-matsen-88b1a8133/
Here are some videos that are of shoulder interest
Shoulder arthritis - what you need to know (see this link).
How to x-ray the shoulder (see this link).
The ream and run procedure (see this link).
The total shoulder arthroplasty (see this link).
The cuff tear arthropathy arthroplasty (see this link).
The reverse total shoulder arthroplasty (see this link).
The smooth and move procedure for irreparable rotator cuff tears (see this link).
Shoulder rehabilitation exercises (see this link).